Translate this page into:
Giant Ulcerating Pilomatricoma: A Case Report
*Corresponding author: Vimal Bheemsain Sangam, Department of Dermatology, Medical College Baroda, Vadodara, Gujarat, India. vimalsangam12@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sangam VB, Patel NM, Shah HA, Chauhan J. Giant Ulcerating Pilomatricoma: A Case Report. Indian J Postgrad Dermatol. 2025;3:39-41. doi: 10.25259/IJPGD_140_2024
Abstract
Pilomatricoma is a rare benign adnexal neoplasm originating from hair follicle matrix cells in which giant, bullous, ulcerating, anetodermic and lymphangiectatic variants may be seen. Giant pilomatricomas (size > 5 cm) rarely ulcerate, and are often a diagnostic challenge as they resemble cutaneous malignancies. We report the case of a 45-year-old male who presented with a slow-growing, ulcerating nodule on the left forearm.
Keywords
Adnexal neoplasm
Hair tumour
Shadow cells
INTRODUCTION
Pilomatricoma, also known as calcifying epithelioma of Malherbe, is a rare benign adnexal neoplasm originating from hair follicle matrix cells, comprising 0.12% of skin tumours. It predominantly affects children and young adults, with a female preponderance.[1] Typically slow growing and well circumscribed, it presents as a cystic or firm nodule measuring 0.5–2 cm, often located on the head and neck, upper extremities and trunk.[2] Rarely, bullous, ulcerating, anetodermic, lymphangiectatic and giant variants occur. Giant pilomatricomas (size > 5 cm) rarely ulcerate, and are often a diagnostic challenge as they resemble cutaneous malignancies.[1] This report aims to highlight one such diagnostic challenge.
CASE REPORT
A 45-year-old male presented with a gradually enlarging mass on his left forearm for 2 months. Physical examination revealed a 5 × 5 cm2 exophytic, centrally firm, tender ulcerated nodule with yellowish crusting on the flexor aspect [Figure 1]. No fixity or discharge was noted, and surrounding skin was unaffected. There was no history of trauma, infection or prior skin cancers; general examination, routine tests and chest X-ray were normal. Dermatoscopy showed irregular whitish streaks, reddish pink areas, bluish grey regions and multiple dotted and few irregular linear vascular patterns [Figure 2]. Differential diagnoses included squamous cell carcinoma, keratoacanthoma, lymphoma, melanoma, sarcoma and metastasis. A 4-mm punch biopsy showed shadow cells, basaloid cells, inflammatory infiltrate and metaplastic calcification foci, suggestive of pilomatricoma. In a small biopsy specimen, evaluating the structure and growth patterns of a neoplasm can be challenging. This difficulty extends to distinguishing between pilomatricoma and pilomatrix carcinoma, as well as discerning between their aggressive and proliferative variants. The lesion was excised under local anaesthesia with histopathological differential diagnoses of aggressive pilomatricoma, proliferating pilomatricoma and pilomatrix carcinoma in mind. Macroscopically, the lesion was clearly defined and had a grey-tan colour. Microscopically, an unencapsulated neoplasm involving the whole dermis, with aggregates of basaloid matrical cells peripherally and eosinophilic shadow cells centrally, which favoured a fully developed pilomatricoma, was present. Foci of metaplastic ossification were seen [Figures 3]. No necrosis, haemorrhage or invasion was observed. Few mitoses were noted. Follow-up showed no complications or recurrence.

- Giant ulcerating pilomatricoma: Erythematous ulcerated nodule with yellowish crusting seen on flexor aspect of the left forearm.
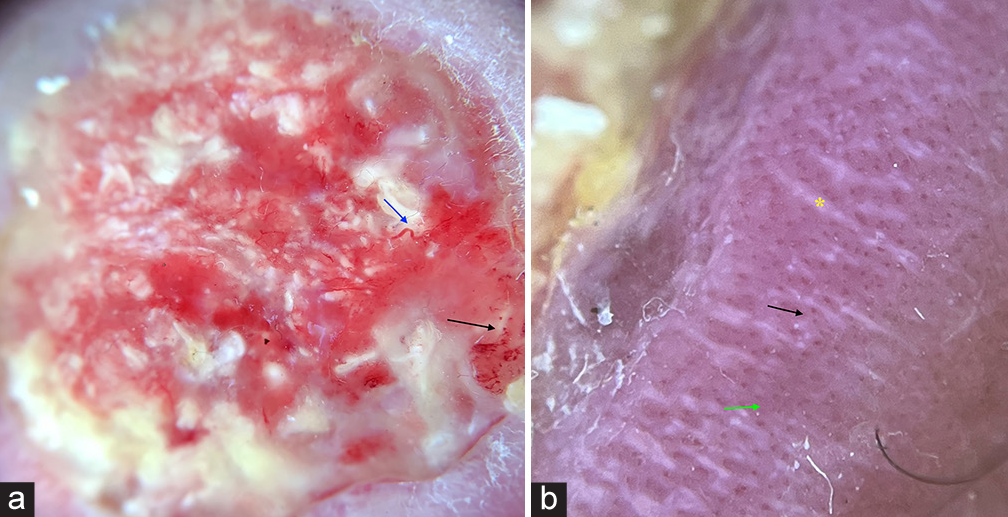
- Dermatoscopy (using dermatoscope IDS-1100, under polarised light with ×10 magnification) in giant ulcerating pilomatricoma showing (a) dotted vessels (black arrow) and linear irregular vessels (blue arrow), (b) irregular whitish streaks (asterix), few reddish pink homogenous areas (green arrow) and dotted vessels (black arrow), IDS: Illuco dermatoscope.
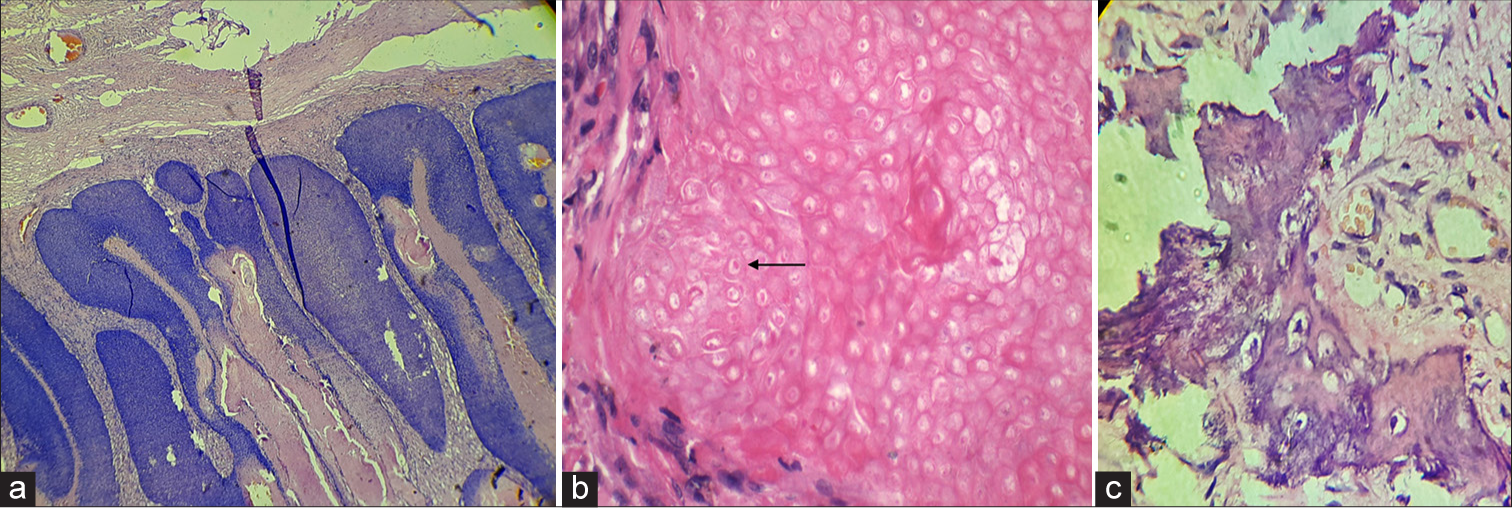
- Histopathology of giant ulcerating pilomatricoma showing (a) well-circumscribed unencapsulated neoplasm involving the whole dermis, composed of aggregates of basaloid matrical cells aligned at the periphery and shadow cells centrally (H&E ×10) (b) shadow cells (black arrow) in H&E ×40 (c) Foci of metaplastic ossification (H&E ×40). H&E: Haematoxylin and eosin.
DISCUSSION
Pilomatricoma, a benign tumour from hair follicle matrix, has been inaccurately diagnosed preoperatively (up to 30% cases) due to its similarity to other tumours.[3] Although its cause is unclear, B-cell lymphoma-2 gene and beta-catenin pathway have been implicated.[4,5] While generally not hereditary, multiple lesions can occur with Gardner’s syndrome, Steinert disease and Turner’s syndrome.[3] Dermatoscopic features include irregular, whitish streaks indicating calcification and cornification, reddish homogeneous zones, hairpin-like, linear irregular and dotted vessels representing vascular structures and structureless grey-blue areas corresponding to melanin within basaloid cell aggregates or siderophages in inflammatory infiltrate.[6-8]
Pilomatricoma features ‘shadow cells,’ a unique microscopic sign of flawed hair differentiation.[9-12] Shadow cells are named so because although their silhouettes are discernible, the nuclei are not observed. They form a characteristic feature of pilomatricoma and are significant because they represent differentiation towards the hair cortex, seen as structureless eosinophilic cells lacking nuclei.[4] Pilomatricomas progress through four stages: (a) Early cystic lesions, (b) fully developed large cysts, (c) early regressive with basaloid cells, shadow cells, lymphocytic infiltrate and multinucleated giant cells and (d) late regressive with numerous shadow cells, no basaloid or inflammatory cells and eventual calcification and ossification.[4,12]
In our case, proliferating pilomatricoma, aggressive pilomatricoma and pilomatrix carcinoma were shortlisted as histopathological differential diagnoses after examination of limited biopsy specimen and diagnosis was confirmed after examination of surgically excised specimen. Proliferating pilomatricomas typically occur around the seventh decade, while aggressive and benign forms are more common in children and young adults.[1,4] Proliferating and aggressive pilomatricomas represent intermediate stages of a histological spectrum between benign pilomatricoma and pilomatrix carcinoma.[4] Our case differed from proliferating pilomatricoma by lacking nuclear atypia and mitotic figures. Aggressive pilomatricomas typically show a higher matrical cell component, increased mitotic activity (7/10 high-power fields [HPF] vs. 1–2/10 HPF), single cell necrosis, prominent nucleoli, invasive growth patterns and nuclear pleomorphism, all absent in our case.[4,11] Pilomatrix carcinoma was ruled out due to the absence of abnormal mitosis, nuclear crowding, pleomorphism, necrosis and lymphatic or perineural invasion.[4,5]
Surgical excision is the preferred treatment for pilomatricomas, with a low recurrence rate (more common in proliferating types). Fixed tumours are excised along with the overlying dermis.[13]
CONCLUSION
Pilomatricomas pose diagnostic challenges due to their histopathological complexity. Giant ulcerating pilomatricomas can mimic malignancies, highlighting the importance of recognising shadow cells, a key histopathological clue essential for accurate pre-operative diagnosis.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Giant Pilomatrixoma: A Distinctive Clinical Variant: A New Case and Review of the Literature. Dermatol Online J. 2020;26:13030/qt4h16s45w.
- [CrossRef] [PubMed] [Google Scholar]
- Giant Pilomatrixoma Arising in the Preauricular Region: A Case Report. Kulak Burun Bogaz Ihtis Derg. 2004;12:147-9.
- [Google Scholar]
- An Unusual Presentation of Giant Pilomatrixoma in An Adult Patient. J Dermatol Case Rep. 2013;7:56-9.
- [CrossRef] [PubMed] [Google Scholar]
- An Ulcerated Giant Pilomatricoma Mimicking Malignancy. J Dtsch Dermatol Ges. 2015;13:329-30.
- [CrossRef] [PubMed] [Google Scholar]
- Ulcerated Giant Pilomatrixoma in a Child. Actas Dermosifiliogr. 2013;104:924-5.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of Pilomatricoma: A Case Report with a Review of the Literature. Our Dermatol Online. 2022;13:82-5.
- [CrossRef] [Google Scholar]
- Giant Proliferating Pilomatricoma; Report of a Rare Entity. Aust J Dermatol. 2017;58:e91-3.
- [CrossRef] [PubMed] [Google Scholar]
- Giant Pilomatrix Carcinoma of the Face. J Oral Maxillofac Surg. 2018;76:368-73.
- [CrossRef] [PubMed] [Google Scholar]
- Giant Pilomatrical Tumor With Broad Epidermal Components: An Example of Histological Diversity and a Potential Diagnostic Pitfall of Tumors With Pilomatrical Differentiation. Am J Dermatopathol. 2022;44:129-134.
- [CrossRef] [PubMed] [Google Scholar]
- Giant Pilomatricoma Mistaken for a Malignant Tumor. J Craniofac Surg. 2023;34:e409-10.
- [CrossRef] [PubMed] [Google Scholar]
- A Case of AA Amyloidosis Complicated by Proliferating Pilomatricoma and a Review of the Literature. J Dermatol. 2024;51:1360-3.
- [CrossRef] [PubMed] [Google Scholar]







