Translate this page into:
Reticular Erythematous Mucinosis: A Case Report and Brief Review
*Corresponding author: Priya Prafulla Kadu, Department of Dermatology, Venerology and Leprosy, Government Medical College, Akola, Maharashtra, India. kadupriya15@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kadu PP, Laul RA. Reticular Erythematous Mucinosis: A Case Report and Brief Review. Indian J Postgrad Dermatol. 2024;2:36-8. doi: 10.25259/IJPGD_95_2023
Abstract
Reticular erythematous mucinosis is a rare entity characterised by mucin deposition in the skin. It has been reported in association with a few autoimmune diseases such as type 1 diabetes mellitus, systemic lupus erythematosus, systemic sclerosis, Hashimoto’s thyroiditis and idiopathic thrombocytopenic purpura. It is commonly misdiagnosed and treated as photodermatitis due to its subtle presentation. The case is being reported due to its rarity.
Keywords
Reticular erythematous mucinosis
Mucin
Autoimmunity
INTRODUCTION
Reticular erythematous mucinosis (REM) is an uncommon primary cutaneous mucinosis characterised by persistent reticular macular erythema or erythematous papules and plaques in the midline of the back or chest. Associations reported with REM are certain malignancies (haematological, breast, lung and colon), thyroid dysfunction, systemic lupus erythematosus, diabetes, idiopathic thrombocytopenic purpura and human immunodeficiency virus. We report a case of REM, which was initially misdiagnosed as photodermatosis due to its rare occurrence.
CASE REPORT
A 52-year-old male presented with redness over the neck, chest and back for 2 years. There was a burning sensation that was exacerbated following sun exposure. There was no history of the application of any drug, fever, joint pain or difficulty in getting up from a sitting position. Family history and past medical history were insignificant. The patient had been treated for photodermatosis using sunscreens, topical steroids, and oral steroids previously, but he did not have any benefit.
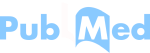
On examination, multiple erythematous papules were present over the neck, chest and upper back [Figure 1a and b]. Oral cavity, genitals, nails and scalp examination were unremarkable.
Complete blood count and liver and renal function tests were within normal limits. Antinuclear autoantibodies were negative. Creatinine kinase type MB level performed to rule out dermatomyositis was normal. Haematoxylin-eosin staining of biopsy specimens of involved skin showed a normal epidermis with mucin deposition in the dermis in between the collagen bundles. A lymphocytic infiltrate was seen in the perivascular region [Figure 1c]. Mucin deposition was confirmed by Alcian blue staining, which was suggestive of REM [Figure 1d]. Direct immunofluorescence tested for immunoglobulin and complement deposition was negative. To determine any underlying associations, fasting and postprandial blood sugar levels, a thyroid profile, ultrasound of the abdomen and X-ray chest were done which were unremarkable. Based on the lesion morphology, distribution and histopathology, a final diagnosis of REM was made.

- Images showing erythematous papules in a reticulate pattern over the (a) neck, chest and (b) upper back, (c) Haematoxylin-eosin-stained section showing a normal epidermis with perivascular lymphocytic infiltrate and marked separation of collagen bundles (×40). (d) Alcian blue staining showing abundant dermal mucin deposition by virtue of the blue colour (×40).
The patient was started on topical sunscreen, oral hydroxychloroquine 200 mg twice daily along with oral prednisolone starting with 30 mg/day and tapered slowly over 12 weeks, with a significant improvement in the symptoms and signs by the end of 2 months [Figure 2a and b]. The patient is on regular follow-up with good control of the disease activity.
- (a and b) Post-treatment images showing resolution of the lesions.
DISCUSSION
REM is a rare mucin deposition disorder with unclear pathogenesis. Proposed aetiologies include viruses, immunological disturbances and solar radiation.[1] X-rays, menses, oral contraceptives, pregnancy and heat are triggers. Asymptomatic or mildly pruritic lesions present as macules, papules and plaques in a reticulate pattern over the chest and back in the midline. Uncommonly, the face, arms, axillae, abdomen, legs and surgical scars may be involved. Although more commonly reported in women, it is also seen in men, as in this case.
On histology, the epidermis is normal, as in our case. Mild spongiosis or lichenoid inflammation has also been described. Mild superficial and mid-dermal perivascular superficial infiltrate is seen. In the perifollicular region, the infiltrate comprises mainly lymphocytic cells, with a few mast cells, histiocytes and factor XIIIa-positive dendrocytes.[1,2] A characteristic finding is the separation of dermal collagen bundles by mucin deposition in the upper and mid-dermis,[3] which was present in our case.
Immunohistochemistry has revealed an accumulation of hyaluronan and this may be related to factor XIIIa+/HAS2+ dermal dendrocytes.[4] Plasmacytoid dendritic (bone marrow-derived CD123 and CD2AP positive) cells have been reported frequently in the lesions of REM,[3] but their role is not well defined. Another study has shown a defective response of fibroblasts to interleukin-1 beta.[5]
Hydroxychloroquine (200–400 mg/day) is a first-line therapy because it results in rapid improvement; however, recurrences are common. Other therapies include topical corticosteroids, topical calcineurin inhibitors, oral steroids, tetracycline, dapsone and cyclosporine. Our patient had a good response to a combination of hydroxychloroquine and oral prednisolone. Ultraviolet A1 (UVA1) radiation and pulsed-dye laser have yielded promising results.[1] UVA1 acts by enzyme induction that results in the breakdown of hyaluronic acid.[1] Pulsed dye laser is effective in reducing the disease activity after 3–5 sessions as it acts by selective thermolysis of vessels at a depth of 1.2–1.5 mm.[1]
REM is closely related to lupus erythematosus tumidus (LET). However, recent studies have concluded that REM is a distinct disease with characteristic midline lesions with firm consistency as opposed to LET which has oedematous lesions with occasional annular configuration.[3] The histological differences include denser and deeper infiltration of lymphocytes and deeper deposition of mucin in LET than in REM.[3]
CONCLUSION
Reticular Erythematous Mucinosis should be considered in all cases of photodermatosis that do not respond to treatment despite photoprotective measures.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Reticular Erythematous Mucinosis--a Review. Int J Dermatol. 2012;51:903-9.
- [CrossRef] [PubMed] [Google Scholar]
- Reticular Erythematous Mucinosis: A Review of Patients' Characteristics, Associated Conditions, Therapy and Outcome in 25 Cases. Br J Dermatol. 2013;169:1207-11.
- [CrossRef] [PubMed] [Google Scholar]
- Reticular Erythematous Mucinosis: Histopathological and Immunohistochemical Features of 25 Patients Compared with 25 Cases of Lupus Erythematosus Tumidus. J Eur Acad Dermatol Venereol. 2015;29:689-97.
- [CrossRef] [PubMed] [Google Scholar]
- Reticular Erythematous Mucinosis Syndrome with an Infiltration of Factor XIIIa+ and Hyaluronan Synthase 2+ Dermal Dendrocytes. Br J Dermatol. 2001;145:141-5.
- [CrossRef] [PubMed] [Google Scholar]
- Reticular Erythematous Mucinosis Syndrome: Glycosaminoglycan Synthesis by Fibroblasts and Abnormal Response to Interleukin-1 Beta. Dermatology. 1996;192:41-5.
- [CrossRef] [PubMed] [Google Scholar]