Translate this page into:
Syphilitic Primary Chancre Mimicking Decubitus Ulcer in Pelvic Organ Prolapse
*Corresponding author: Taru Garg, Department of Dermatology, Lady Hardinge Medical College, New Delhi, India. tarugarg4@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Sahu A, Garg T. Syphilitic Primary Chancre Mimicking Decubitus Ulcer in Pelvic Organ Prolapse. Indian J Postgrad Dermatol. 2025;3:66-7. doi: 10.25259/IJPGD_112_2024
Dear Editor,
Syphilis is a sexually transmitted infection (STI) caused by Treponema pallidum. Primary syphilis manifests as a painless ulcer known as a chancre, which typically occurs at the site of infection.[1] Pelvic organ prolapse (POP) is the protrusion of the pelvic organs into the vagina.[2] Sometimes, it is complicated by the development of decubitus ulcer, a common complication of advanced POP, due to venous congestion resulting in oedema of the surrounding tissue. The presence of this ulceration leads to delay in surgical management such as hysterectomy further affecting the quality of life of the patient.[3] The presence and size of these ulcers are correlated with the stage of POP, with larger ulcers more common in advanced stages.[4] We herein present a unique case of a syphilitic primary chancre mimicking a decubitus ulcer in a patient with uterine prolapse.
A 38-year-old female was referred from antiretroviral therapy centre, with complaints of a foul-smelling discharge and discomfort in her genital area for the past 2 weeks. The patient denied any history of premarital or extramarital contacts, drug abuse, blood transfusion and tattooing. Last unprotected penovaginal sexual contact with husband was 1 year back. The husband was truck driver by occupation and living separately most of the time. She had a history of uterine prolapse for many years for which she had not sought medical attention previously. On examination, she was found to have a stage IV uterine prolapse, with the cervix protruding approximately 5 cm beyond the introitus. In addition, a single well-defined painful ulcer of 2 × 2 cm2, with erythematous and indurated base, was present on the prolapsed part without any associated evidence of venous congestion [Figure 1a]. Inguinal lymphadenopathy was not evident.
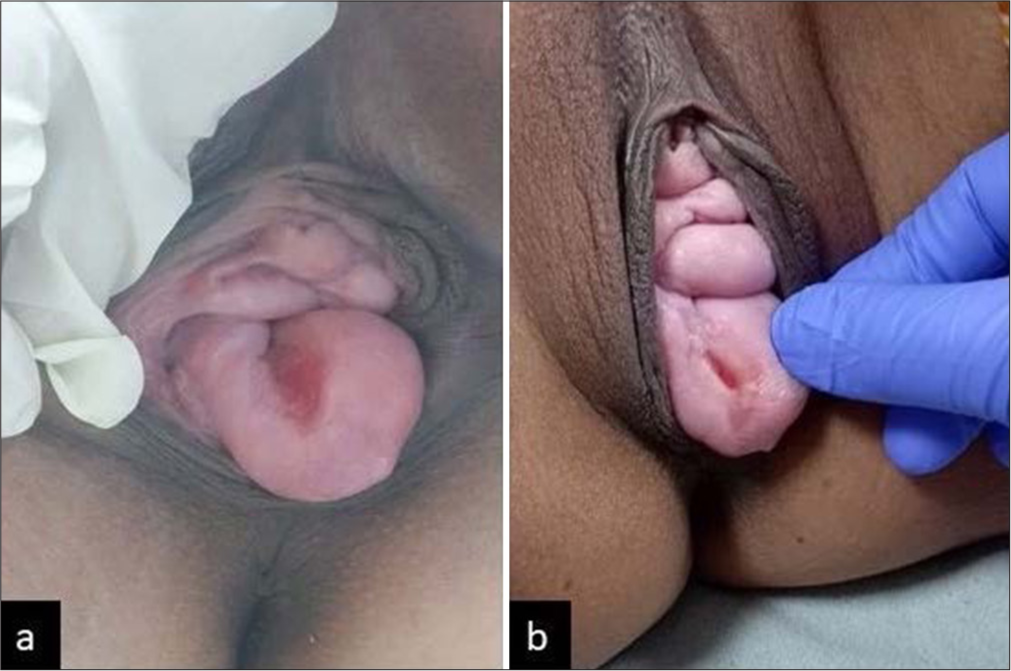
- (a) Single ulcer with indurated base before treatment, (b) Healed ulcer after treatment.
Given the appearance of the lesion, history of high-risk behaviour in husband and seropositive status, further investigations were undertaken. Serological tests for syphilis, including venereal disease research laboratory test with titres: 1:32, and T. pallidum haemagglutination test were positive. No evidence of any intraepidermal lesion or malignancy was found on the Papanicolaou smear examination.
The patient was diagnosed with primary syphilis and was treated with single injection of benzathine penicillin, 2.4 million units, deep intramuscular. She was also counselled on safe sexual practices and the importance of partner testing and treatment. During follow-up visit at 7 days, the ulcer healed completely [Figure 1b].
Primary syphilitic chancres typically occur on the external genitalia or anus, or mouth, depending upon the type of sexual contact with an infected individual. In females, cervix is commonly involved site. However, because of painless nature of the ulcer and deeper location, this is commonly missed.[1] Further, in rare cases, chancres may develop in atypical locations or present with unusual features and may lead to missed diagnosis.[5] Our patient was also misdiagnosed initially as decubitus ulcer because of location of the ulcer on prolapsed part. Possibility of malignancy was also considered by the gynaecologist, and the patient was referred to us due to her seropositive status to rule out any STIs. This highlights the need for a high index of suspicion for STIs, in such scenario for prompt diagnosis and treatment, and to prevent the progression of syphilis to its secondary and tertiary stages.
Even though primary chancre on cervix uteri is a common finding, its resemblance to a decubitus ulcer within the context of uterine prolapse has not been reported previously. Healthcare providers should maintain vigilance for such presentations and promptly investigate and treat such patients appropriately.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Syphilis: A Commentary on Current Literature. Sex Transm Infect. 1928;4:310-7.
- [CrossRef] [Google Scholar]
- Pelvic Organ Prolapse In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK563229 [Last accessed on 2024 Jun 13]
- [Google Scholar]
- Decubitus Ulcers among Women with Uterovaginal Prolapse. J Womens Health Care. 2018;7:433.
- [Google Scholar]
- Study of the Relationship between Pelvic Organ Prolapse Quantification (POP-Q) Staging and Decubitus Ulcer in Pelvic Organ Prolapse. Cureus. 2021;13:e12443.
- [CrossRef] [Google Scholar]
- Syphilis: Uncommon Presentations in Adults. Clin Dermatol. 2005;23:555-64.
- [CrossRef] [PubMed] [Google Scholar]






