Translate this page into:
Reversible Hyperpigmentation due to Vitamin B12 Deficiency - Mimicking Addison’s Pigmentation
*Corresponding author: Yogindher Singh, Department of Dermatology, Sri Venkateshwaraa Medical College Hospital and Research Centre, Puducherry, India. yogindher@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Vijay V, Ahmed M, Singh Y. Reversible Hyperpigmentation due to Vitamin B12 Deficiency - Mimicking Addison’s Pigmentation. Indian J Postgrad Dermatol. 2024;2:42-4. doi: 10.25259/IJPGD_116_2023
Abstract
Vitamin B12 deficiency, which is usually seen in vegetarians, is characterised by cutaneous, gastrointestinal, neurological and haematological manifestations. Cutaneous manifestations include hyperpigmentation, glossitis and hair changes. Hyperpigmentation seen in Vitamin B12 deficiency mimics Addison’s disease. Here, we present a case of a 65-year-old male with vitamin B12 associated hyperpigmentation, which improved with B12 supplementation.
Keywords
Vitamin B12 deficiency
Hyperpigmentation
Addisonian pigmentation
INTRODUCTION
Addisonian pigmentation is defined as generalised hyperpigmentation commonly involving the photo-exposed sites, flexures and mucosal areas.[1] Causes of generalised hyperpigmentation include excessive sun exposure, drugs, Addison’s disease and nutritional disorder such as Vitamin B12 deficiency. Vitamin B12 deficiency, first reported by Dr. Bramwell Cook in 1944, is characterised by macrocytic anaemia, glossitis and cutaneous hyperpigmentation. Here, we report a case of a 65-year-old male with hyperpigmentation over acral sites for 4 months.
CASE REPORT
A 65-year-old male came to the outpatient department of dermatology with complaints of generalised fatigue and hyperpigmentation over the body × 4 months. There was no history of photosensitivity or drug intake. The patient did not have any neurological symptoms. He was a known case of diabetes mellitus and was on irregular medications. He was a vegetarian, non-smoker and non-alcoholic. On examination, there was diffuse hyperpigmentation predominantly seen over the face, bilateral forearms, lower legs, palms and soles [Figure 1]. Oral cavity showed greyish-black hyperpigmentation of the buccal mucosa [Figure 2]. Longitudinal melanonychia was seen over the fingernails [Figure 1b]. Sensory examination was normal. Dermoscopy (Heine’s 30, ×10 magnification, non-polarised mode) showed brown reticular areas forming a pseudonetwork-like pattern around eccrine gland openings [Figure 3a]. His serum Vitamin B12 levels were 18.5 pg/mL (normal 187–883 pg/mL). Serum cortisol levels were normal (12 μg/dL). Other blood investigations such as complete haemogram, serum ferritin, liver function test and serum folic acid levels were normal. A 4-mm punch biopsy was taken from the left forearm and sent for histopathological examination. Haematoxylin and eosin-stained section showed hyperkeratosis, mild acanthosis with elongation of rete ridges, increased melanin in the basal layer and pigment incontinence in the superficial dermis [Figure 3b and c]. Based upon these findings, the patient was diagnosed with Addisonian pigmentation due to Vitamin B12 deficiency and was started an injection Vitamin B12 (1000 mcg) intramuscularly daily for 1 week followed by injection Vitamin B12 1500 mcg intramuscularly weekly once for 4 weeks followed by 1500 mcg monthly once for 3 months. The pigmentation improved significantly in 12 weeks [Figures 2 and 4] along with normalisation of serum Vitamin B12 levels. The patient has been advised of dietary modifications and is currently on Vitamin B12 tablets (1500 mcg).

- (a) Hyperpigmentation over flexor aspect of forearms and palms. (b) Hyperpigmentation over extensor aspect of forearms, dorsum of both hands with nails showing longitudinal melanonychia. (c) Hyperpigmentation over anterior aspect of lower legs and dorsum of feet. (d) Hyperpigmentation over posterior aspect of lower legs.

- (a and b) Hyperpigmentation over bilateral buccal mucosa. (c and d) Resolution of hyperpigmentation after treatment.
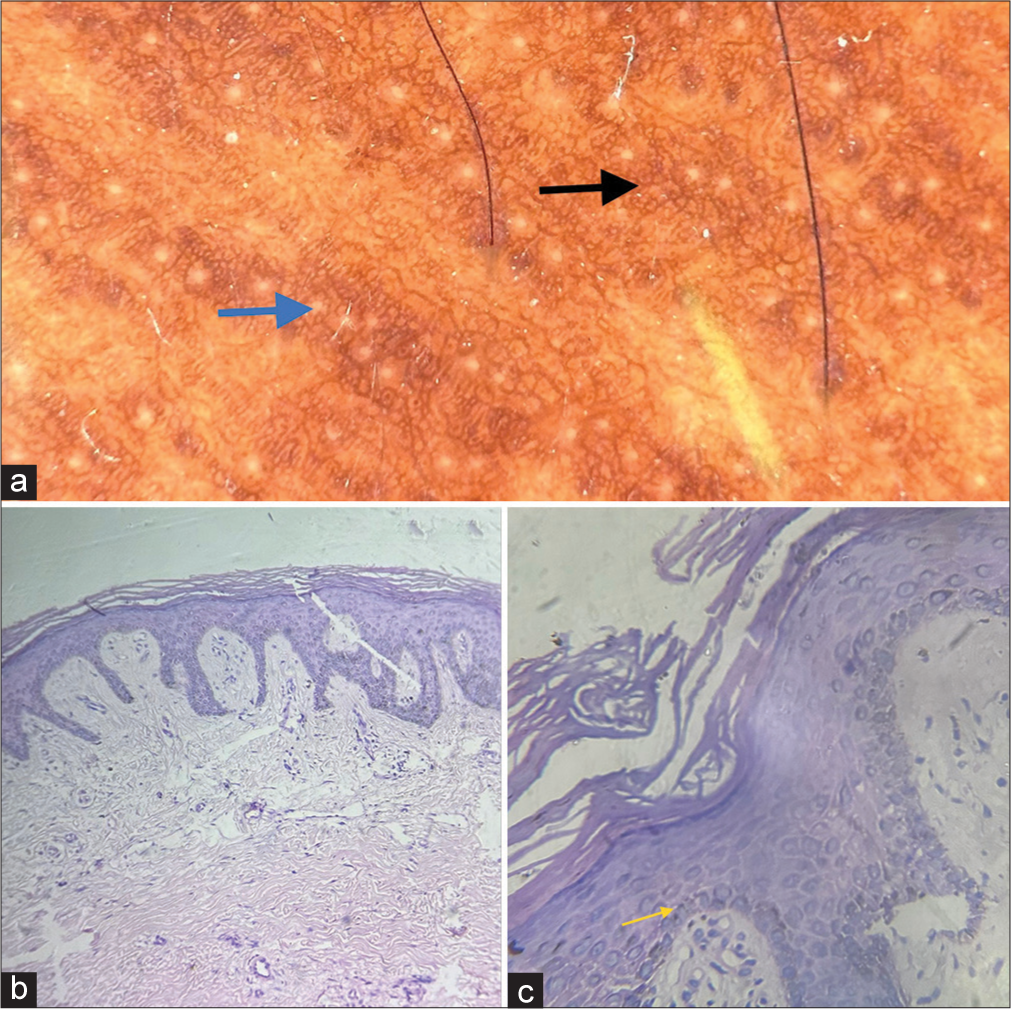
- (a) Dermoscopy (Heine’s 30, 10× magnification, nonpolarised mode) shows brown reticular areas forming a pseudo network like pattern (black arrow) around eccrine gland openings (blue arrow). (b) Hematoxylin and eosin-stained section – 10× view shows hyperkeratosis, mild acanthosis with elongation of rete ridges, increased melanin in the basal layer. (c) Hematoxylin and eosin-stained section – 40× view shows magnified image of hyperkeratosis, acanthosis, increased melanin in the basal layer (yellow arrow) and pigment incontinence in superficial dermis.
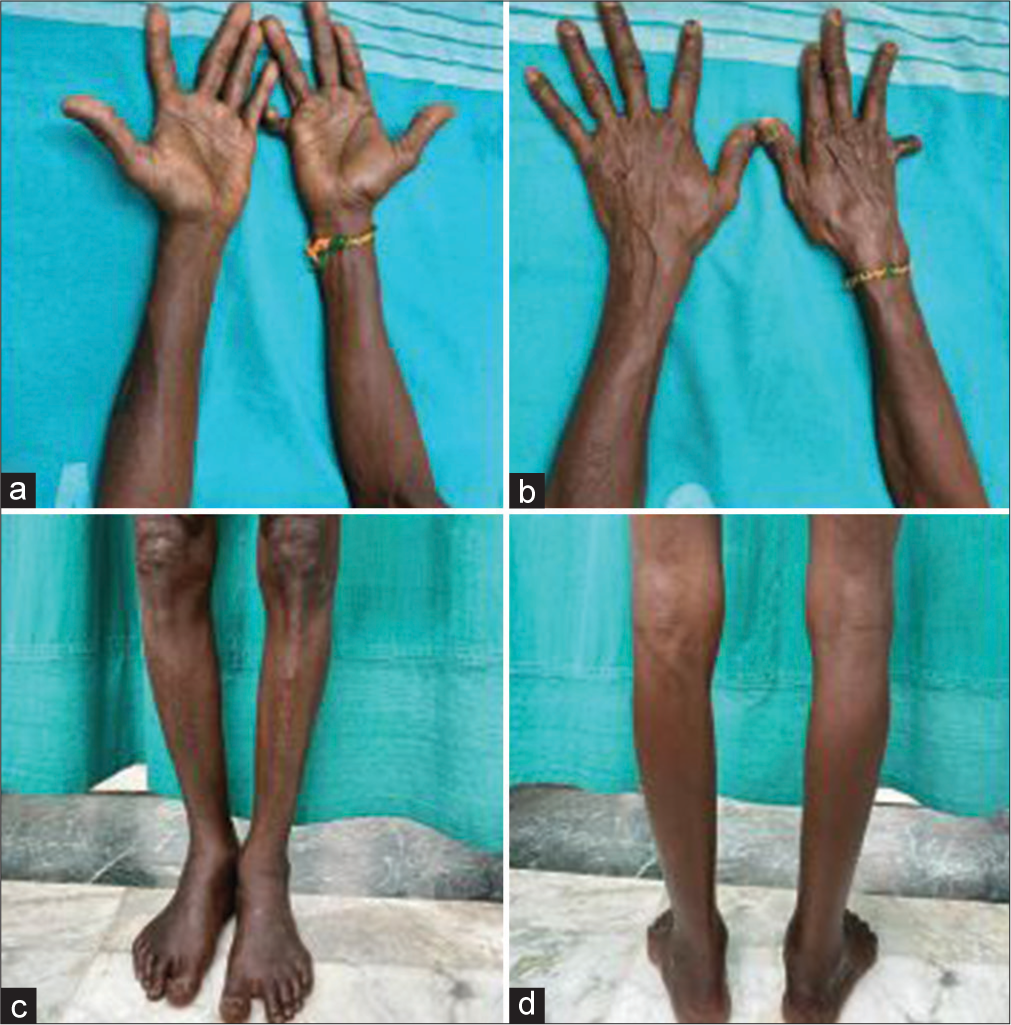
- (a) Post treatment reversal of hyperpigmentation over flexor aspect of both forearms and palms. (b) Post treatment reversal of hyperpigmentation over extensor aspect of both forearms and dorsum of hands. (c) Post treatment reversal of hyperpigmentation over anterior aspect of both lower legs and feet. (d) Post treatment reversal of hyperpigmentation over posterior aspect of both lower legs and feet.
DISCUSSION
Vitamin B12 is a water-soluble vitamin that cannot be synthesised by humans. The dietary source of Vitamin B12 is through consumption of meat, fish, eggs, cheese and dairy products. The recommended dietary allowance of B12 is about 1 mcg/day. Deficiency of B12 occurs due to inadequate intake, decreased consumption of meat and dairy products, low intrinsic factor and malabsorption due to gastrectomy. Mucocutaneous manifestations include hyperpigmentation, angular stomatitis, hair changes (greying, textural changes) and vitiligo.[2] Hyperpigmentation is the main presenting feature of Vitamin B12 deficiency.[3] Hyperpigmentation is usually seen over the acral sites, especially dorsum of hands and feet, palms, soles, nails and oral cavity. It has been noted in previous studies that 1 in 5 people with Vitamin B12 deficiency have hyperpigmentation.[3] It can also be the only presentation of Vitamin B12 deficiency.[3] Hyperpigmentation in B12 deficiency occurs as a result of (1) decreased levels of reduced glutathione which activates tyrosinase and results in increased melanin synthesis, (2) defect in transfer of melanin from melanocytes to keratinocytes resulting in pigment incontinence, (3) increased biopterin in B12 deficiency increases hydroxylated phenylalanine which results in hyperpigmentation. The systemic features of B12 deficiency are fatigue, loss of weight, loss of appetite and glossitis.[2] Neurological manifestations include subacute combined degeneration of the spinal cord and peripheral neuropathy (in the form of glove and stocking paraesthesia and trichodynia).[1] Investigations include a complete haemogram, microbiologic/radio-assay of plasma or serum Vitamin B12 and shillings test. Histopathological examination of skin biopsy shows epidermal atrophy, increased melanin in the basal layer and pigment incontinence.[2] Treatment for Vitamin B12 deficiency consists of oral and/or parenteral Vitamin B12 based on the clinical severity.[3] The time taken for resolution of cutaneous hyperpigmentation varies from 6 to 12 weeks.[3]
CONCLUSION
Addisonian pigmentation due to Vitamin B12 deficiency is not a common occurrence. Early diagnosis and prompt treatment prevents the development of neurological complications which are usually irreversible. High index of suspicion should be present among physicians when a vegetarian patient presents with hyperpigmentation over the body.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Addisonian Pigmentation Responding to Vitamin B12: The Nails Tell the Story! Dermatol Ther. 2022;35:e15187.
- [CrossRef] [Google Scholar]
- Pigmentation in Vitamin B12 Deficiency Masquerading Addison's Pigmentation: A Rare Presentation. Indian J Endocrinol Metab. 2013;17:S254-6.
- [CrossRef] [PubMed] [Google Scholar]
- Hyperpigmentation as a Primary Symptom of Vitamin B12 Deficiency: A Case Report. Cureus. 2022;14:e29008.
- [CrossRef] [Google Scholar]







