Translate this page into:
Idiopathic Localised Perforating Calcinosis Cutis Over the Bilateral Distal Phalanx of the Middle Finger - A Rare Case Report
*Corresponding author: Aparna Thirumalaiswamy, Department of Dermatology, Venereology and Leprology, Seth GSMC and KEM Hospital, Mumbai, Maharashtra, India. taparna97@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Thirumalaiswamy A, Khade P, Gole PV, Salve MJ, Mahajan SA. Idiopathic Localised Perforating Calcinosis Cutis Over the Bilateral Distal Phalanx of the Middle Finger - A Rare Case Report. Indian J Postgrad Dermatol. 2024;2:45-7. doi: 10.25259/IJPGD_77_2023
Abstract
Calcinosis cutis or cutaneous calcification occurs when calcium is deposited into the skin and subcutaneous tissue. It is classified into five primary types: Dystrophic, metastatic, idiopathic, iatrogenic and calciphylaxis. Idiopathic calcinosis cutis is a rare phenomenon that occurs in the absence of a known tissue injury or systemic metabolic defect. The various types of idiopathic calcinosis are idiopathic calcinosis of scrotum/penis/vulva, milia-like idiopathic calcinosis cutis, subepidermal calcified nodule, tumoural calcinosis, localised calcinosis cutis and calcinosis universalis. It is essential to delineate it from other calcification disorders for further plan of management. We report one such case of idiopathic localised perforating calcinosis cutis, symmetrically over a bilateral distal phalanx of the middle finger in a 72-year-old female.
Keywords
Calcinosis cutis
Down’s syndrome
Phospholipids
Raynaud’s phenomenon
INTRODUCTION
Calcinosis cutis is an uncommon disorder characterised by abnormal deposition of calcium phosphate in the skin and frequently presents with diagnostic hurdles due to its rarity. We present a case of idiopathic calcinosis cutis in a 72-year-old female, highlighting its occurrence in an elderly individual and its unique bilaterally symmetrical presentation.
CASE REPORT
A 72-year-old female, devoid of known comorbidities, presented to the dermatology department with asymptomatic, multiple, yellowish-white nodules on the bilateral distal phalanx of her middle fingers. The lesions had been present for 5 years, originating on the distal phalanx of the right middle finger and subsequently noticed in the left middle finger within 6 months. Some nodules occasionally discharged chalky material. There was no history of local trauma, prior infections or excessive calcium/phosphate intake. The patient denied symptoms such as proximal muscle weakness, joint pain, photosensitivity or skin tightening. Cutaneous examination revealed symmetrical diffuse swelling of the bilateral distal phalanx of the middle fingers, with multiple ill-defined, yellowish-white, fixed, hard deposits beneath the skin’s surface [Figure 1a and b]. Pinpoint shallow ulcers with purulent crusted floors were observed on the palmar surface of the bilateral middle finger distal phalanges. Notably, no such depositions were evident on the other fingers, elbows, buttocks or any other sites. On examination, the nails were normal and the distal phalyngeal joints had normal range of motion. Systemic and musculoskeletal examinations yielded normal results.

- (a) Multiple, yellowish-white nodules on the bilateral distal phalanx of the middle finger (b) Multiple pinpoint shallow ulcers with brown crust on the distal phalanx right middle finger.
A skin biopsy taken from the pad of the right middle finger revealed hyperkeratosis and acanthosis of the epidermis, along with a zone of amorphous, basophilic, homogenous deposits in the dermis [Figure 2a]. Von Kossa staining confirmed these deposits as calcium [Figure 2b]. On higher magnification, trans-epidermal elimination of the basophilic material was noticed [Figure 2c].
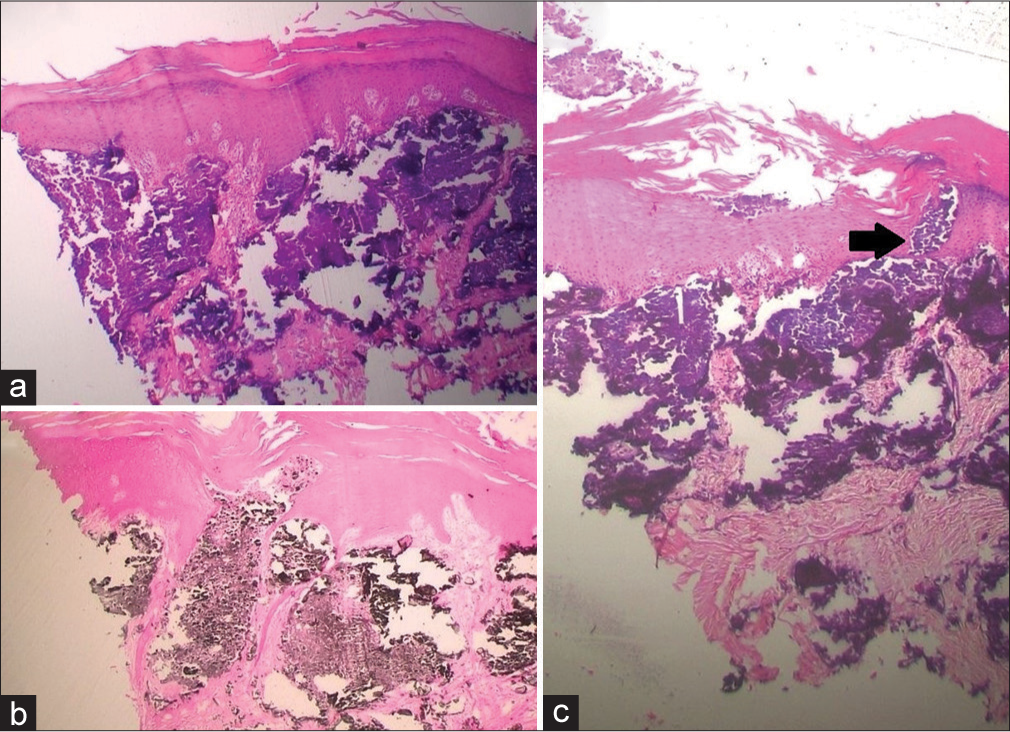
- (a) Acanthotic epidermis with dermal deposit of basophilic material (H&E, ×4), (b) Positive Von Kossa silver stain suggesting deposits of calcium in dermis and stratum corneum (Von Kossa, ×4), (c) Transepidermal elimination of basophilic material from dermis depicted by black arrow (H&E, ×20).
Local X-ray of the bilateral hand demonstrated homogenous white deposition in the pad of the distal phalanx of the bilateral middle finger [Figure 3a and b].

- (a) X-ray of the right hand (homogenous white deposition in pad of the distal phalanx of bilateral middle finger) (b) X-ray of the left hand (homogenous white deposition in pad of the distal phalanx of bilateral middle finger).
Serum calcium and phosphorous levels, renal function tests, serum parathyroid hormone levels, anti-nuclear antibody assay, muscle enzymes and serum Vitamin D levels were all within normal limits.
Based on clinical, laboratory, histopathological and radiological findings, perforating idiopathic calcinosis cutis was diagnosed.
The patient was given topical 20% sodium thiosulphate (STS) under occlusion, but unfortunately, due to loss of follow-up, the response could not be assessed.
DISCUSSION
Hydroxyapatite crystals or amorphous calcium phosphate accumulation in the skin and subcutaneous tissue is the hallmark of calcinosis cutis.[1] It is classified into five primary types based on its aetiology: Dystrophic, metastatic, iatrogenic, calciphylaxis and idiopathic.[1,2] Idiopathic calcinosis cutis is an uncommon condition that does not have any recognised tissue damage or internal metabolic disorders.[3] The exact pathogenesis is yet unknown, however, it is postulated that dysfunction in gamma carboxy glutamic acid (GCGA) metabolism leads to the accumulation of GCGA in skin and tissues, facilitating calcium phosphate deposition.[3,4]
It is divided into six main clinical types: Calcinosis universalis (discharging hard nodules and plaques), subepidermal calcified nodule (hyperkeratotic, tender, usually solitary nodule on the extremities and eyelids), localised idiopathic dermal calcinosis, tumoural calcinosis, scrotal calcinosis and milia-like idiopathic calcinosis cutis (seen in Down syndrome).[5]
In contrast to our case, which happened in an elderly patient, idiopathic calcinosis cutis typically affects children and adolescents.[1,2] Histopathological examination of calcinosis cutis shows a focus of calcium in the dermis and subcutaneous tissue, which is confirmed using the Von Kossa stain. Perforation may or may not be present.[4] Finger-tip calcinosis cutis is usually associated with systemic sclerosis, Raynaud’s phenomenon and CREST syndrome. Similar cases of fingertip calcinosis cutis patients with scleroderma have been reported in the literature.[6,7] However, our patient had no systemic symptoms, and there were no signs of trauma or inflammatory process in the lesion with normal laboratory data.
Differentials of hard nodules on the fingers include enchondromas and osteochondromas. These are usually found in the younger age group and can be differentiated from calcinosis cutis based on radiographic findings. Osteochondromas (exostoses) present as sessile projections from the underlying metaphyses of the bone, while enchondromas present as expansile lytic lesions arising from the medullary cavity of the underlying bone.[8]
Improving blood flow to the extremities and avoiding stress, exposure to the cold and trauma are general therapeutic methods for treating calcinosis cutis. While more widespread diseases will need medical management, patients with minor, localised lesions are ideal candidates for surgical treatments such as excision and carbon dioxide laser.[3] Even though no medication has been shown to be effective in clinical trials, there are currently a number of treatment options available, including intravenous immunoglobulin, warfarin, bisphosphonates, minocycline, calcium channel blockers (most commonly diltiazem), ceftriaxone, aluminium hydroxide, probenecid, biologics such as infliximab and rituximab and intralesional steroids.[3] STS in intravenous, intralesional and topical formulations has also been studied as a treatment for calcinosis cutis.
CONCLUSION
Idiopathic calcinosis cutis, though a rare entity, should be kept under suspicion even in the case of the elderly population. It is essential to rule out a history of trauma, chronic kidney disease, excessive intake of calcium or phosphates supplements, parathyroid anomalies and connective tissue disorders in the elderly before initiating treatment.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Idiopathic Calcinosis Cutis over Elbow in a 12-Year Old Child. Case Rep Orthop. 2013;2013:241891.
- [CrossRef] [PubMed] [Google Scholar]
- Unilateral Idiopathic Calcinosis Cutis: A Case Report. Case Rep Dermatol. 2017;9:20-4.
- [CrossRef] [PubMed] [Google Scholar]
- Milia-like Idiopathic Calcinosis Cutis in a Child with Down Syndrome. Dermatol Online J. 2016;22:13030/qt7080c5gs.
- [CrossRef] [Google Scholar]
- A Case of Idiopathic Calcinosis Cutis. Med J Armed Forces India. 2012;68:383-5.
- [CrossRef] [PubMed] [Google Scholar]
- Generalized Milia-like Calcinosis Cutis in a Child with Down Syndrome: Dermoscopic Features. Dermatol Online J. 2021;27:13030/qt0bx294gm.
- [CrossRef] [PubMed] [Google Scholar]
- Successful Treatment of Calcinosis Cutis of Fingertip in the Setting of CREST Syndrome with Topical 20% Sodium Thiosulfate. JAAD Case Rep. 2019;5:988-90.
- [CrossRef] [PubMed] [Google Scholar]
- Fingertip Calcinosis Cutis in an Incomplete Limited-type Systemic Scleroderma. Eur J Dermatol. 2011;21:797-8.
- [CrossRef] [PubMed] [Google Scholar]
- Enchondroma of the Hand. J Am Acad Orthop Surg. 2016;24:625-33.
- [CrossRef] [PubMed] [Google Scholar]







