Translate this page into:
Hypotrichosis-Lymphoedema-Telangiectasia Syndrome: Brief Report and Literature Review
*Corresponding author: Yasmeen Jabeen Bhat, Department of Dermatology, Venereology and Leprosy, Govt Medical College, Srinagar, Jammu and Kashmir, India. yasmeenasif76@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ul Islam M, Bhat YJ, Binti Ismail I. Hypotrichosis-Lymphoedema-Telangiectasia Syndrome: Brief Report and Literature Review. Indian J Postgrad Dermatol. 2024;2:31-5. doi: 10.25259/IJPGD_89_2023
Abstract
Hypotrichosis-lymphoedema-telangiectasia syndrome (HLTS) can be identified by defects in the superficial vasculature, lymphatic system and hair follicles. We report a case of a 25-year-old female who presented with sparse hair throughout the scalp, body, eyebrows, nasal telangiectasia and oedema of the lower limbs. Once the patient is diagnosed with HLTS, lifelong monitoring of vascular integrity is essential.
Keywords
Hypotrichosis
Lymphoedema
Telangiectasia
SOX18
INTRODUCTION
Hypotrichosis-lymphoedema-telangiectasia syndrome (HLTS), an extremely rare hereditary disease, can be identified by defects in the superficial vasculature, lymphatic system and hair follicles with diverse phenotypic variability. The syndrome has been linked to a mutation in the SOX18 gene and can rarely involve cardiac and renal systems.[1,2] To date, only a few cases have been reported in the literature. Here, we report a case of a 25-year-old female with suspected HLTS.
CASE REPORT
A 25-year-old female presented with increased shedding, roughness and non-growing scalp hair for the last 15 years. The patient also provided a history of swelling of both legs for the same period and recurrent episodes of epistaxis over the past 3 years. Her mother and father were related through a second-degree consanguineous marriage. Cutaneous examination revealed her hair as thin, coarse, fragile and sparse throughout her scalp [Figure 1a and b]. Reduced density of body hair, and eyebrows was also noted. On anterior rhinoscopy, telangiectasias were seen in the Kiesselbach’s triangle [Figure 1c] and pitting oedema [Figure 1d] in the lower limbs. Her nails and teeth were normal. Trichoscopic examination revealed thin, fine, curled and predominantly single hair shafts without any evidence of inflammation (×10, DL4) [Figure 2a]. Examining the hair shaft under a light microscope revealed dystrophic anagen hair root with cuticle weathering [Figure 2b]. The only abnormalities detected throughout laboratory tests were a microcytic hypochromic blood picture, hypoproteinemia and hypoalbuminemia. The kidney function test and echocardiography were normal. Abdominal ultrasound revealed minimal ascites, mild splenomegaly and a right-sided pleural effusion. Doppler ultrasonography of the lower extremity revealed only a few fibrinous strands in the saphenous vein. Magnetic resonance lymphangiography revealed diffuse epiphyseal oedema involving bilateral legs with a prominent lymphatic channel showing a torturous and beaded appearance along the lateral aspect of the distal end of the right leg, measuring 3.2 mm in calibre lying at a distance of 6.6 mm from the skin surface [Figure 3]. Rest of the systemic analysis was unremarkable. Based on the above findings, a diagnosis of HLTS was made.

- (a and b) Thin, coarse, and sparse hair throughout the scalp. (c) Telangiectasias seen in the Kiesselbach’s triangle (black arrow). (d) Pitting oedema in the lower limbs.
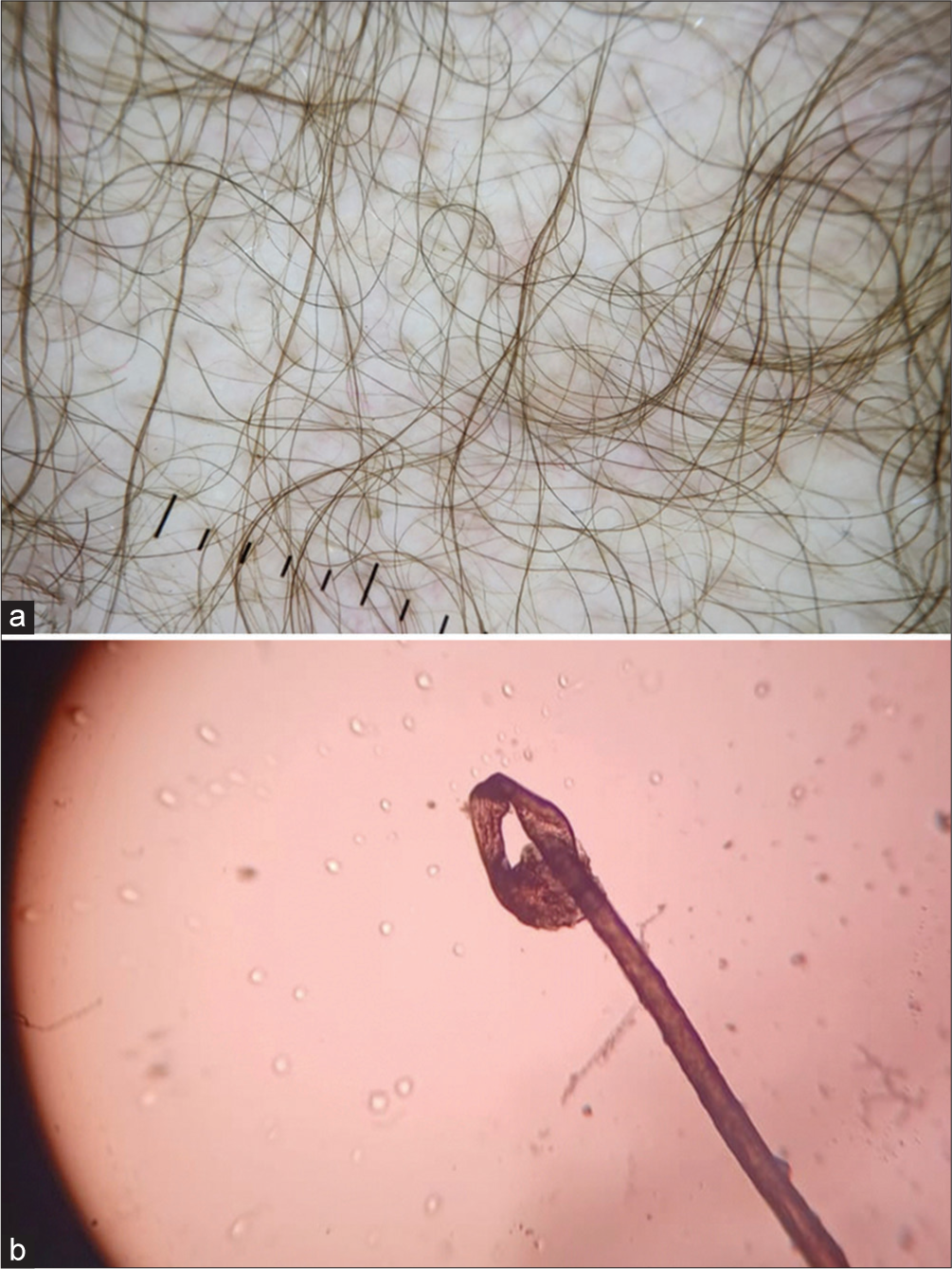
- (a) Trichoscopic examination revealing thin, fine, curled and predominantly single hair shafts without any evidence of inflammation (×10, DL4). (b) Light microscopy revealing dystrophic anagen hair root with cuticle weathering.

- Magnetic resonance lymphangiography revealing diffuse epiphyseal oedema involving bilateral legs with a prominent lymphatic channel showing a torturous and beaded appearance along the lateral aspect of the distal end of the right leg, measuring 3.2 mm in calibre lying at a distance of 6.6 mm from the skin surface.
DISCUSSION
Hair disorders can be inherited, or they might arise as people age. Here, we reported a case of an acquired hair disorder with lymphoedema and telangiectasia. Our differentials included hair shaft disorders with syndromic associations and we excluded them as there was no ectodermal dysplasia, keratosis pilaris, atopy, ichthyosis linearis circumflexa and neuroectodermal changes. HLTS has been linked to a mutation in the transcription factor gene SOX18. Irrthum et al. reported five cases with recessive or dominant SOX18 mutations in 2003, when HLTS was first described. The SOX18 gene encodes a transcriptional activator that is important for the development of specific tissues, including the blood vessels, hair follicles and lymphatic systems.[2-4] HLTS appears to be caused by two distinct types of SOX18 variants: missense mutations that impact the HMG box (recessive inheritance) and non-sense mutations that result in shortened proteins without the transactivation activity (dominant inheritance).[5,6] Hypotrichosis, lymphoedema and telangiectasias of varying severity can occur in HLTS patients. Other features may include renal failure, aortic dilatation, a large nasal root, prognathism, swollen eyelids and a dysmorphic face. Renal disease might appear several years after HLTS diagnosis and tends to be progressive. Clinical features observed in 13 HLTS patients, 12 reported by other authors, are documented in Table 1.[2,3,7] In addition to the hair problems, our patient also had lymphatic system development complications, which manifested as lower limb oedema. There were also nasal telangiectasias caused by defects in the development of vascular systems.[7] As HLTS involves a multidisciplinary approach, the patient was referred to the ear, nose and throat department, where she underwent cauterisation of dilated vessels, and the cardiovascular thoracic surgery department for further management. However, the patient was lost to follow-up.
| S No. | Case | Gender M/F | Hypotrichosis | Lymphatic dysfunction | Hydrocele | Telangiectasia | Facial dysmorphism | Epistaxis | Nail abnormality | Arterial hypertension | Kidney dysfunction | Non-immune hydrops fetalis | Aortic dilatation |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Case I | F | + | + | − | + | + | − | − | − | − | − | − |
| 2. | Case II | M | + | + | + | − | − | − | − | − | − | − | − |
| 3. | Case III | F | + | + | − | + | − | − | − | − | − | − | − |
| 4. | Case IV | M | − | + | − | − | − | − | − | − | − | + | − |
| 5. | Case V | M | + | + | + | + | + | + | − | + | + | − | − |
| 6. | Case VI | M | + | + | + | + | + | + | − | + | + | − | − |
| 7. | Case VII | F | + | − | − | + | − | + | + | + | − | − | + |
| 8. | Case VIII | M | + | + | − | + | + | − | + | − | − | + | − |
| 9. | Case IX | M | + | + | − | − | + | − | − | − | − | − | − |
| 10. | Case X | M | + | + | + | + | − | − | − | − | − | − | − |
| 11. | Case XI | M | + | + | + | + | + | + | + | − | + | + | + |
| 12. | Case XII | F | + | − | − | + | − | − | − | − | − | − | − |
| 13. | Present case | F | + | + | − | + | − | + | − | − | − | − | − |
HTLS: Hypotrichosis-lymphoedema-telangiectasia syndrome
Limitations
Whole exome sequencing was not done in our patient due to financial constraints. Hence, we encourage further studies with mutation analysis to detect novel variants and genotype-phenotype correlation.
CONCLUSION
HLTS is characterised by a wide range of symptoms that majorly impact the hair, vascular and lymphatic systems. Once the HLTS diagnosis has been established, patient’s vascular integrity should be carefully monitored throughout their life. Monitoring for renal impairment, pulmonary hypertension and aortic dilatation should be considered.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- A Novel SOX18 Mutation Uncovered in Jordanian Patient with Hypotrichosis-Lymphedema-Telangiectasia Syndrome by Whole Exome Sequencing. Mol Cell Probes. 2016;30:18-21.
- [CrossRef] [PubMed] [Google Scholar]
- Mutations in the Transcription Factor Gene SOX18 Underlie Recessive and Dominant Forms of Hypotrichosis-Lymphedema-Telangiectasia. Am J Hum Genet. 2003;72:1470-8.
- [CrossRef] [PubMed] [Google Scholar]
- Hypotrichosis-Lymphedema-Telangiectasia Syndrome: Report of Ileal Atresia Associated with a SOX18 de novo Pathogenic Variant and Review of the Phenotypic Spectrum. Am J Med Genet A. 2021;185:2153-9.
- [CrossRef] [PubMed] [Google Scholar]
- Vascular Defects in a Mouse Model of Hypotrichosis-Lymphedema-Telangiectasia Syndrome Indicate a Role for SOX18 in Blood Vessel Maturation. Hum Mol Genet. 2009;18:2839-50.
- [CrossRef] [PubMed] [Google Scholar]
- Construction and Functional Analysis of Novel Dominant-negative Mutant of Human SOX18 Protein. Biochemistry (Mosc). 2013;78:1287-92.
- [CrossRef] [PubMed] [Google Scholar]
- Hypotrichosis-Lymphedema-Telangiectasia-Renal Defect Associated with a Truncating Mutation in the SOX18 Gene. Clin Genet. 2015;87:378-82.
- [CrossRef] [PubMed] [Google Scholar]
- A Case with Hypotrichosis-Lymphedema-Telangiectasia Syndrome with Hair Shaft Fragility. Skin Appendage Disord. 2022;8:511-4.
- [CrossRef] [PubMed] [Google Scholar]







