Translate this page into:
Cervical Spine Involvement: A Rare Entity in Psoriasis
*Corresponding author: Aarti Avinash Zope, Department of Rheumatology, Bliss Clinic, Thane, Maharashtra, India. aarti_zope@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Zope AA, Patil SP. Cervical Spine Involvement: A Rare Entity in Psoriasis. Indian J Postgrad Dermatol 2023;1:124-6.
Dear Sir,
We hereby present a case of a 42-year-old male, known case of psoriasis for 7 years on treatment, who presented with complaints of inflammatory low back pain for the past 10 years and gradually progressive limitation of neck movement for the past 4 years. There was no history of peripheral joint involvement, no history suggestive of dactylitis or uveitis or inflammatory bowel disease. On examination, our patient was obese, without any evidence of peripheral arthritis or enthesitis or nail changes. He had axial involvement in the form of limited lumbar spinal mobility (Schobers~1 cm and Chest expansion~2.5 cm); limited cervical spine mobility (Neck flexion~10°, Extension~10°, Lateral rotation~15° and Lateral flexion~10°). Psoriatic patches were seen over trunk and both legs [Figure 1] with Psoriasis Area Severity Index (PASI~10). Systemic examination was normal. Drug history included cyclosporine with initial relief in skin lesions and some over the counter non-steroidal anti-inflammatory drugs (NSAIDs) with partial relief in pain and stiffness. His investigations revealed loss of cervical lordosis, vertebral squaring, diffuse osteopenia, fusion of posterior elements and syndesmophytes (bilateral bridging symmetrical) on cervical spine X-ray [Figure 2]; while X-ray lumbosacral spine showed vertebral squaring with diffuse osteopenia with few syndesmophytes. Erythrocyte sedimentation rate (ESR) was 98, C-reactive protein (CRP) 12.7; human leucocyte antigen B27 (HLA-B27) by flow cytometry was negative. Pre-biologic screening was negative. He was hence diagnosed as psoriatic arthritis (PsA) with predominant axial involvement (with baseline PASI~10, Bath-Ankylosing-Spondylitis-Disease-Activity-Index [BASDAI]~4.8). Considering high disease activity for axial disease and skin involvement refractory to conventional therapy, he was started on Inj Adalimumab s/c 80 mg and 40 mg alternate every 2 weeks and other supportive treatment. His symptoms improved drastically after 6 weeks of treatment. Pain and stiffness resolved up to 80%. Response to treatment with biological disease-modifying antirheumatic drugs (bDMARDs) is assessed after 12 weeks of therapy and is defined as achieving low disease activity (LDA)/remission or at least 50% of improvement in scores.[1] In our case, patient achieved the target and responded well to bDMARD therapy with improvement of BASDAI to 1 and PASI 75 was achieved [Figure 3 and Table 1]. The prevalence of inflammatory arthritis is increased among patients with psoriasis ranging from 7% to 42%.[2] The prevalence of axial involvement (psoriatic spondylitis) varies between 7% and 32% in PsA patients.[3] Tumour necrosis factor (TNF) alpha inhibitors are commonly used in axial spondyloarthropathy (SpA) patients refractory to conventional therapy. Use of interleukin 17 (IL-17) inhibitors is preferred in SpA patients with associated psoriasis. Use of methotrexate or other conventional synthetic disease modifying anti-rheumatic drugs (csDMARDs) in psoriasis helps with peripheral arthritis, but results in axial disease are conflicting. Risk factors for spinal involvement in PsA patients are severe peripheral arthritis, HLA-B27 positivity, radiographic damage to peripheral joints, elevated ESR and presence of nail dystrophy.[4] Spinal involvement in PsA tends to be more spotty and asymmetric; with paravertebral ossification or chunky syndesmophytes; with frequent cervical spine involvement. Asymmetrical sacroiliitis is more common in PsA patients than in ankylosing spondylitis (AS). In a study conducted by El Maghraoui et al., risk of cervical spine involvement was observed to be strongly associated with disease duration, symptomatic severity parameters (Schober, Chest expansion, Bath-Ankylosing-SpondylitisMetrology-Index, Bath-Ankylosing-Spondylitis-Functional-Index and BASDAI) and structural severity parameters (Bath-Ankylosing-Spondylitis-Radiology-Index and Lumbar syndesmophyte score).[5] Early detection of PsA patients will lead to early initiation of specific therapy, which may in turn lead to prevention of long-term morbidity associated with the disease. EULAR treatment guidelines for management of PsA advise use of NSAIDs in predominant axial disease. In cases with failure to achieve target of LDA/Remission in 4 weeks of continuous use of NSAIDs, use of bDMARDs should be considered; as csDMARDs have no proven role in axial disease.[1] Among bDMARDs, either TNF alpha inhibitors (Adalimumab) or IL-17 inhibitors (Secukinumab) can be used. However, as long-term efficacy and safety of IL-17 inhibitors in axial SpA are limited; TNF alpha inhibitors are preferred.
| Index | Pre-bDMARD | 12 weeks after bDMARD |
|---|---|---|
| BASDAI | 4.8 (s/o active disease) | 1 (>50% improvement) |
| ASDAS-ESR | 5.78 (s/o Very High Disease Activity) | 1.94 (>50% improvement) |
| PASI | 10 | PASI 75 achieved (PASI~1.2) |

- (a and b) Skin lesions before therapy.
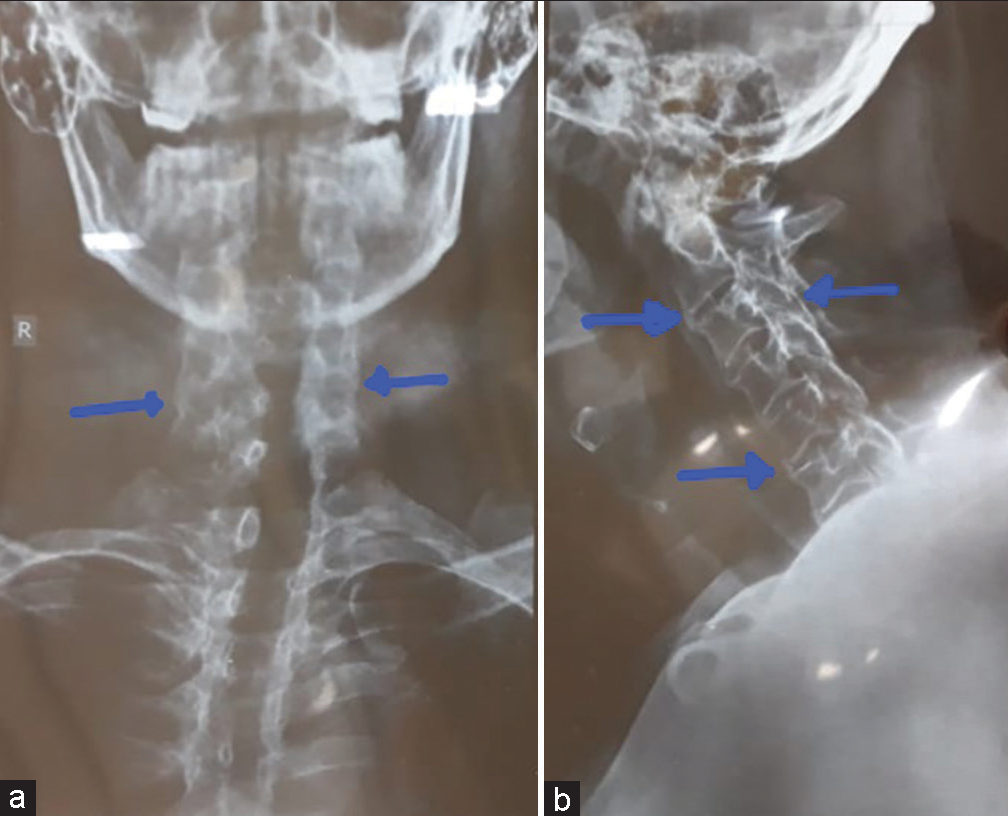
- (a and b) X ray cervical spine (AP and Lateral views) show bilateral bridging syndesmophytes, facet joint ankylosis and loss of cervical lordosis.

- (a and b) Skin lesions after therapy.
Early detection of SpA in psoriasis patients is necessary to prevent long-term morbidity associated with advanced disease. Screening by dermatologists should include presence of inflammatory back pain and restriction in spinal mobility measured by modified Schober’s test and chest expansion on examination. Early referral to a Rheumatologist is needed if joint involvement is suspected. The case presented here is a rare involvement of cervical spine in PsA and role of dermatologists in screening psoriasis patients for axial involvement.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- EULAR Recommendations for the Management of Psoriatic Arthritis with Pharmacological Therapies: 2019 Update. Ann Rheum Dis. 2020;79:700-12.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriatic Arthritis: Epidemiology, Clinical Features, Course, and Outcome. Ann Rheum Dis. 2005;64(Suppl 2):ii14-7.
- [CrossRef] [PubMed] [Google Scholar]
- The Epidemiology of Psoriatic Arthritis. Rheum Dis Clin North Am. 2015;41:545-68.
- [CrossRef] [PubMed] [Google Scholar]
- Risk Factors for Axial Inflammatory Arthritis in Patients with Psoriatic Arthritis. J Rheumatol. 2010;37:809-15.
- [CrossRef] [PubMed] [Google Scholar]
- Cervical Spine Involvement in Ankylosing Spondylitis. Clin Rheumatol. 2003;22:94-8.
- [CrossRef] [PubMed] [Google Scholar]






