Translate this page into:
Basics of Dermoscopy for Beginners
*Corresponding author: Keshavmurthy A. Adya, Department of Dermatology, Venereology and Leprosy, Shri B M Patil Medical College Hospital and Research Centre, BLDE (Deemed to be University), Vijayapura, Karnataka, India. adya.murthy@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Adya KA, Inamadar AC. Basics of Dermoscopy for Beginners. Indian J Postgrad Dermatol. doi: 10.25259/IJPGD_206_2024
QUESTIONS
-
As a diagnostic tool, dermoscopy can
Confirm the clinical diagnosis
Refute the clinical diagnosis and suggest/provide an alternate diagnosis
Narrow down the differential diagnoses
All of the above
-
Dermoscopy is useful in all of the below except
Locating a desired site for biopsy for optimal histopathological outcome
Monitoring the changes in a lesion that may occur over time
Determining the precise resection margins in skin malignancies
Assessing the treatment response
-
Dermoscopy allows visualisation of structures as deep as ___ microns.
10
100
1000
10000
-
Following is not a type of illumination mode in a dermoscope
Polarised light
Non-polarised light
Blue light
None of the above
-
The role of interface fluid is to
Reduce the surface reflection
Make the surface structures more prominent
Make the deeper structures more prominent
Make the pigmented structures more prominent
-
Disadvantage(s) of contact dermoscopy is/are
Possible transmission of infection
Blood vessels may not be properly visualised
Both A and B
Cannot be performed without interface fluid
-
True about polarised illumination dermoscopy
Helps in clearer visualisation of deeper structures
Cuts off surface glare
Does not require interface fluid routinely thus obviating the need for contact dermoscopy
All of the above
-
Deeper structures are best visualised with ___.
Polarised illumination
Non-polarised illumination
Polarised illumination with interface fluid
Non-polarised illumination with interface fluid
-
Following are visualised only in polarised illumination except
Shiny white orthogonal lines
Polychromatic structureless areas (Rainbow phenomenon)
Four-dotted clods (White rosettes)
Follicular keratotic plugs (comedo-like structures)
-
Not true about ‘structures’ in dermoscopy
Structure is an element that has a definite shape and size
Structures can have different morphologies
Morphology of a structure reflects the tissue involved in the pathology
Repeats of a structure form the pattern
-
In the depiction below, which is not a structure?
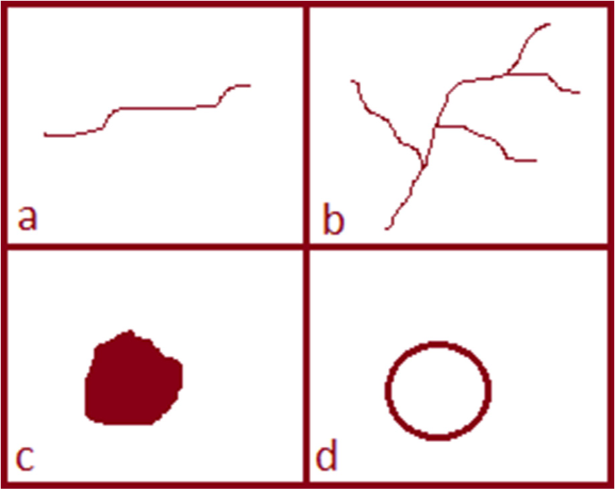
a
b
c
d
-
The primary colours observed in dermoscopy are determined by
The basic chromophores in the skin
The refractive index (RI) of stratum corneum
Degree of hydration of the skin
All of the above
-
Which of the following is not a basic chromophore in the skin?
Keratin
Melanin
Carotene
Haemoglobin
-
The colour imparted by melanin in dermoscopy depends on
Its amount
Its type (eumelanin or pheomelanin)
The size of the melanosomes
The level at which it is located
-
The colour imparted by keratin in dermoscopy depends on
Amount of hyperkeratosis
Type of hyperkeratosis (compact orthokeratotic or non-compact parakeratotic)
Being admixed with serum, blood, melanin, etc.
All of the above
-
White colour in dermoscopy may be due to?
Dermal fibrosis
Calcinosis
Absence/reduction in melanin
All of the above
-
Colours associated with a vascular lesion may be all except
Red
Bluish-black
Greyish-black
Brown
-
The colour imparted by deoxygenated blood in dermoscopy would be
Grey
Dusky red
Bluish-black
Brown
-
Black colour in dermoscopy is imparted by
Melanin
Thrombosed blood vessel
Both
Neither
-
Brown colour of melanin in dermoscopy reflects its location in
Stratum corneum
The Malpighian layer
Papillary dermis
Reticular dermis
-
Melanin in upper reticular dermis appears in dermoscopy as
Black
Grey
Bluish-grey
Bluish-black
-
In dermoscopic parlance, ‘pigmented lesion’ refers to a
Lesion with exogenous pigments such as due to tattooing, heavy metal poisoning, etc.
Melanocytic and/or melanotic lesion
Vascular lesion
Xanthomatous lesion
-
Which dermoscopic pattern among the following is the MOST related to a pigmented lesion?
Pigmented clods and globules
Structureless pigmented areas (pigment blotches)
Pigment lines in reticular pattern (pigment network)
Circumferential or segmental radiating lines with rounded tips (pseudopods)
-
Advantages of using descriptive terminologies for documenting dermoscopic features are all except
Universally comprehendible
Easy to do
Gives the description of the features ‘as is’
Interpretation is not influenced by minor variations in the dermoscopic features
-
False about using metaphoric terminologies in documenting dermoscopic features
Universally incomprehensible
Lengthy and tedious job
Depends on one’s imagination and perception
Interpretation can be influenced by minor variations in the dermoscopic features
ANSWERS
1. d
The essential role of dermoscopy as a diagnostic tool is to add an extra edge to the routine clinical diagnostic exercise for skin lesions. Most of the times, dermoscopy asserts or compliments the clinical diagnosis. On occasions, it might refute the clinical diagnosis and suggest an alternate diagnosis. For some lesions, the dermoscopic diagnostic criteria have been well-established by robust studies which serve conclusive for diagnosis and thereby refute the need for an invasive biopsy. Finally, the list of clinical differential diagnoses following dermoscopy gets certainly narrowed as even if a specific diagnosis is not provided, dermoscopy will give an idea of the tissue involved in the pathology and rule out many unrelated disorders that would have been considered clinically.[1]
2. c
Apart from the primary diagnostic role, dermoscopy is also indispensable in periodic monitoring skin lesions (e.g. a dysplastic nevus), to assess the treatment response and in dermoscopy-directed biopsy for a fruitful outcome, especially in larger lesions [Figure 1]. Although assessment of perilesional area in skin malignancies may provide some subtle clues of extension, dermoscopy cannot precisely delineate the resection margins.[1]

- Illustration of dermoscopy directed biopsy in a case of basal cell carcinoma.
3. b
Using polarised illumination, one can visualise features as deep as 100 microns which levels at the upper to mid reticular dermis.[2]
4. d
Apart from the primary polarised and non-polarised illumination modes, pigment boost, blue light and ultraviolet illuminations are also available in many current-day dermoscopes.[1,3]
5. a
The three essential principles of dermoscopy are illuminating the skin lesion, enhancing the penetration of the illuminated light and magnification of the light reflected from the skin surface and sub-surface region. While the illumination and magnification are provided by light source and achromatic lenses, respectively, penetration of the incident light on the skin surface into the skin is aided by an interface fluid (such as ultrasound probe gel). In dermoscopy, we come across three interfaces – faceplate of the dermoscope (glass) with a RI of 1.52, the intervening air (RI = 1) and the stratum corneum (RI = 1.55). As the intervening air has a lower RI compared to that of stratum corneum, most of the light incident from the dermoscope gets reflected back or scattered. The use of an interface fluid (with RI closer to that the stratum corneum) reduces the surface reflection and provides with more of the light entering into the skin enabling clearer and sharper visualisation of the features [Figure 2].[4]
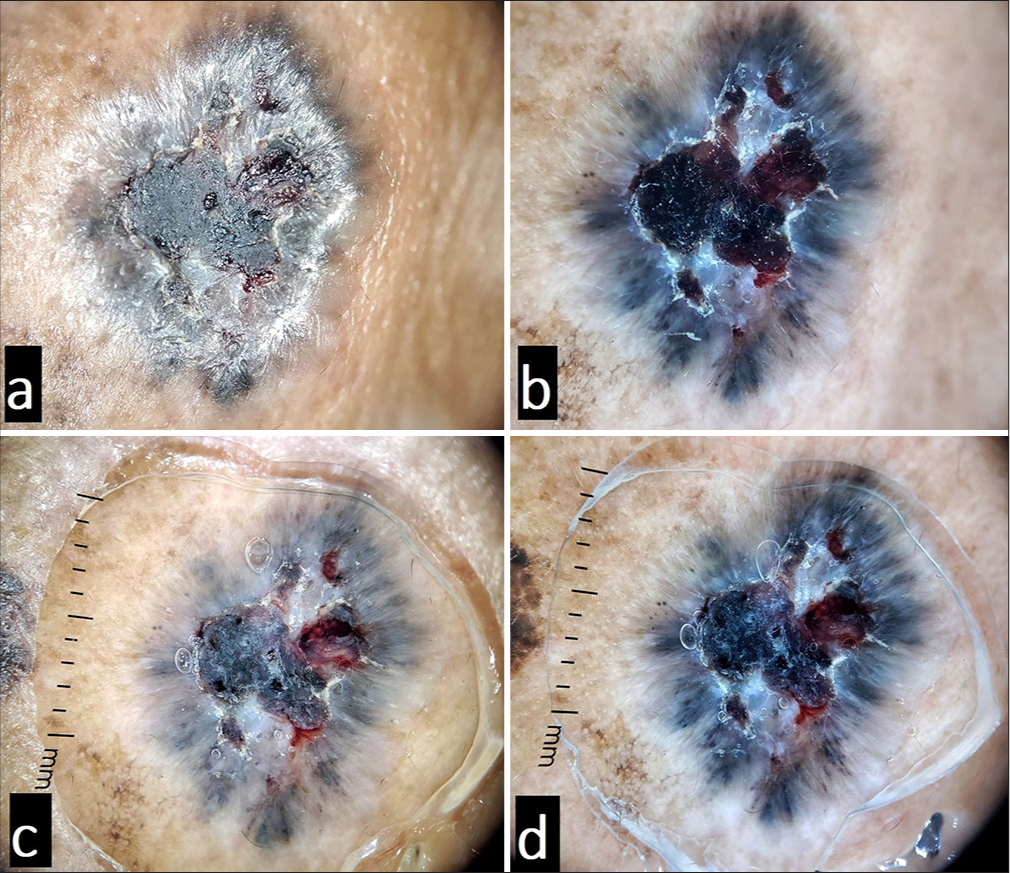
- Illustration of the role of immersion fluid in dermoscopy. Panels (a and b) show non-polarised and polarised views, respectively, without linkage fluid. Panels (c and d) show nonpolarised and polarised views, respectively, with the use of linkage fluid. Polarised dermoscopy allows clearer visualisation of deeper structures while the non-polarised mode makes the surface features clearly visible. Note how the use of linkage fluid reduces the surface reflection (compare a and c). As the light from the dermoscope is trapped in the fluid, the use of linkage fluid also provides sharper views in both polarised mode (as more of the light is available for penetration into the skin) and non-polarised mode as compared to without using it (compare a and c, and b and d).
6. c
Contact dermoscopy refers to the technique of visualisation of lesional features with the faceplate of the dermoscope in direct contact with the skin surface. Apart from the obvious risk of infection transmission, the visibility of vessels may be hampered due to the compressive force that blanches the vessels. Although the use of an interface fluid increases the clarity and resolution of the features, it is not an absolute necessity.[4]
7. d
Polarised illumination dermoscopy employs a source polariser and a detector polariser. The source polariser polarises the light form the source. A part of this light reflects back from the surface while the rest penetrates into the skin and undergoes scattering before getting reflected back. The detector polariser only allows this scattered light reflecting from the skin sub-surface region to enter the eye piece of the dermoscopy while cutting off the surface reflected light. Thus polarised dermoscopy achieves two things – cutting off the surface glare to a greater extent and allowing clearer visualisation of the deeper structures [Figure 2]. Although the use of an interface fluid further enhances the clarity and resolution (refer answer 5), it is not an absolute necessity.[5]
8. c
Refer answers 5 and 7, and Figure 1.
9. d
Apart from clear visualisation of the deeper structures (refer answer 7), polarised dermoscopy exclusively shows certain peculiar features due to optical phenomena. These structures can be seen in many benign and malignant lesions and include the shiny white structures (dots, clods, lines, streaks and structureless areas), four-dotted clods (white rosettes) and polychromatic structureless areas (rainbow phenomenon) [Figure 3]. The shiny white structures (previously called as chrysalis structures) and four-dotted clods (a form of shiny white structure) are seen due to the interaction of polarised light with collagen fibres that have inherent birefringent properties. The polychromatic structureless areas are attributable to the phenomenon of dichroism. A follicular keratotic plug being a skin surface feature is seen with both polarised and non-polarised illumination, although clearer with non-polarised illumination [Figure 4].[5-7]
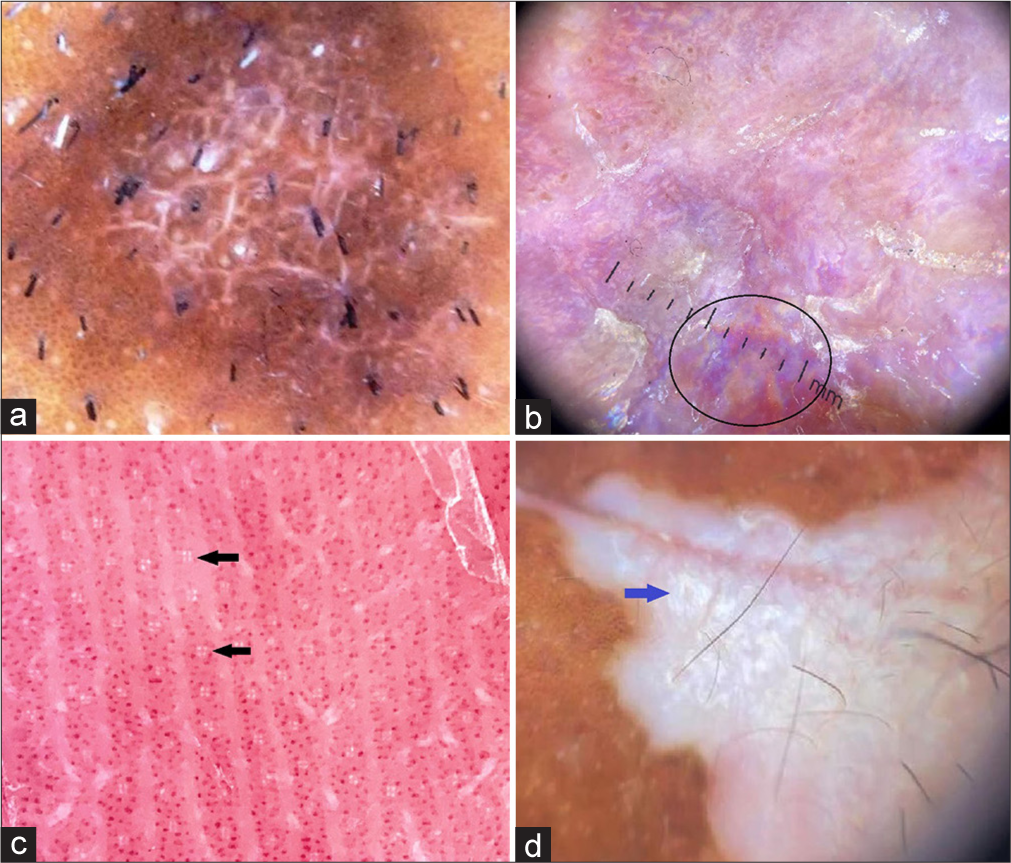
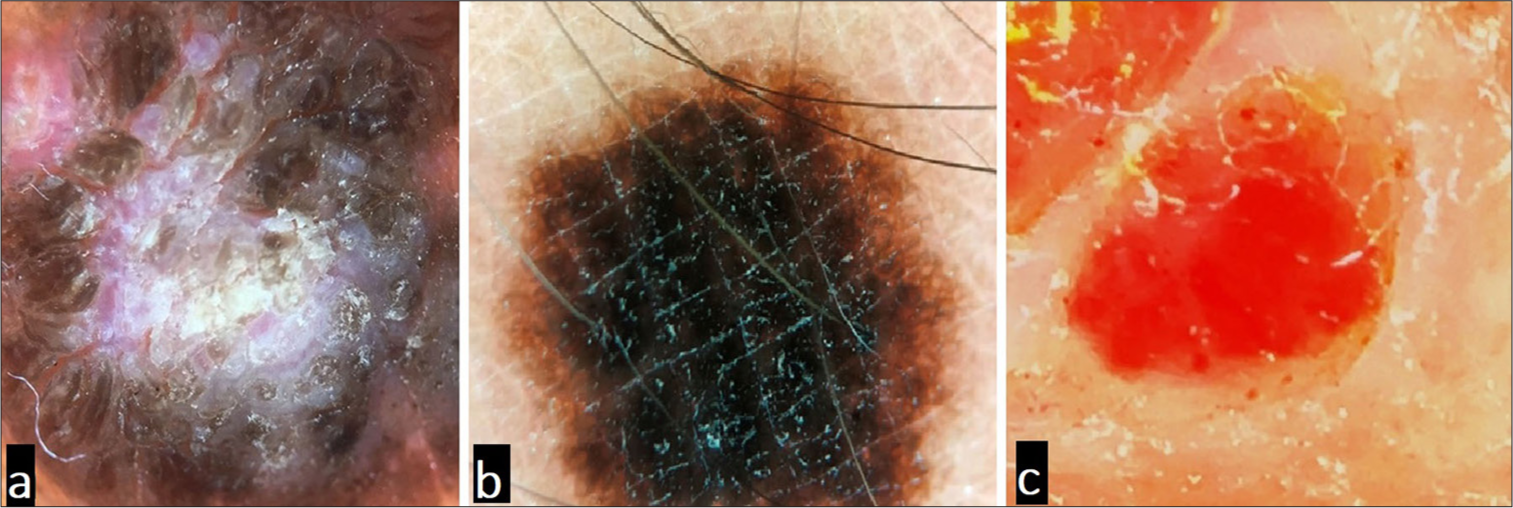
- Illustration of optical phenomena specific to polarised dermoscopy: (a) shiny white lines, (b, black circle) polychromatic structureless area, (c, black arrows) four-dotted clods and (d, blue arrow) shiny white structureless areas.
- Comedo-like structures (yellow arrows) in seborrheic keratosis “visible both in (a) non-polarised and (b) polarised modes. Being surface features, these structures appear more prominent in non-polarised mode.
10. c
‘Structures’ in dermoscopy (lines, dots, clods, circles and pseudopods) are elements with definite shape and size which may have different morphologies (e.g. a ‘line’ may be straight, curved, looped, coiled, helical, etc.). Multiples of a structure form various patterns (e.g. multiple intersecting lines form the ‘reticular pattern’). The main dermoscopic determinant of tissue involved in the pathology is the colour of the structures as they represent the main tissue chromophores in the skin (refer answer 12).[8]
11. b
Panels a, c and d in the diagram show the basic structures. Panel b depicts a branching pattern formed by repeats of the lines (refer answer 10).[8]
12. a
Colours in dermoscopy are possibly the main diagnostic determinants of a lesion. The primary colours observed in dermoscopy are white, black and red imparted by the basic chromophores – keratin, melanin and haemoglobin, respectively [Figure 5]. In practice however, it is important to be aware of two things: (1) The primary colours may not always be depicted by the three basic chromophores (e.g. white colour also represents fibrosis, calcinosis or absence of melanin pigment [Figure 6]; black colour can also be due to thrombosed vessel [refer answer 17 below]) and (2) we observe different colours emitted by the primary chromophores due to various factors such as level of the chromophore (e.g. melanin can appear black, brown, grey and bluish-black when located in the stratum corneum, Malpighian layer, papillary dermis and reticular dermis, respectively [Figure 7]), biological state of the chromophore (e.g. oxygenated and deoxygenated haemoglobin appear bright red and blue-black, respectively) or the amount (e.g. compact orthokeratotic keratin appears yellowish-white and sparse parakeratotic keratin appears white). Hence, it is of paramount importance to interpret the colours in dermoscopy contextually.[3,8]
- Basic chromophores in the skin: (a) keratin – primarily imparting white color, (b) melanin – primarily imparting black color, and (c) hemoglobin – primarily imparting red color.
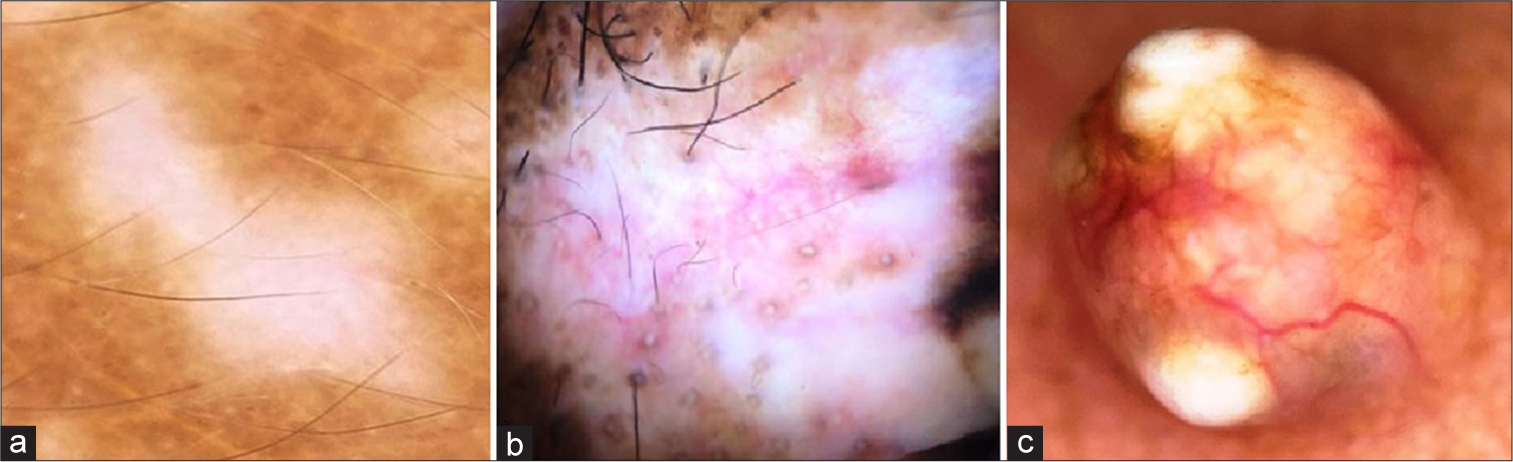
- White color in dermoscopy due to (a) amelanosis in vitiligo, (b) dermal fibrosis in lichen sclerosus, and (c) calcinosis in pilomatricoma.

- Illustration of various colors of melanin in dermoscopy based on its location: (a) black in stratum corneum, (b) brown in Malphigian layer, and (c) gray (white arrow) and blue (yellow arrow) colors due to its presence in papillary and reticular dermis, respectively.
13. c
Refer answer 12.
14. d.
Refer answer 12.
15. d
Apart from the yellow and white colours of keratin due to its amount and type of hyperkeratosis (refer answer 12), keratin may appear yellow-orange, red, black or brown being admixed with serum, fresh blood, deoxygenated blood or melanin and haemosiderin or dirt, respectively.[3]
16. d
Refer answer 12 and Figure 3.
17. c
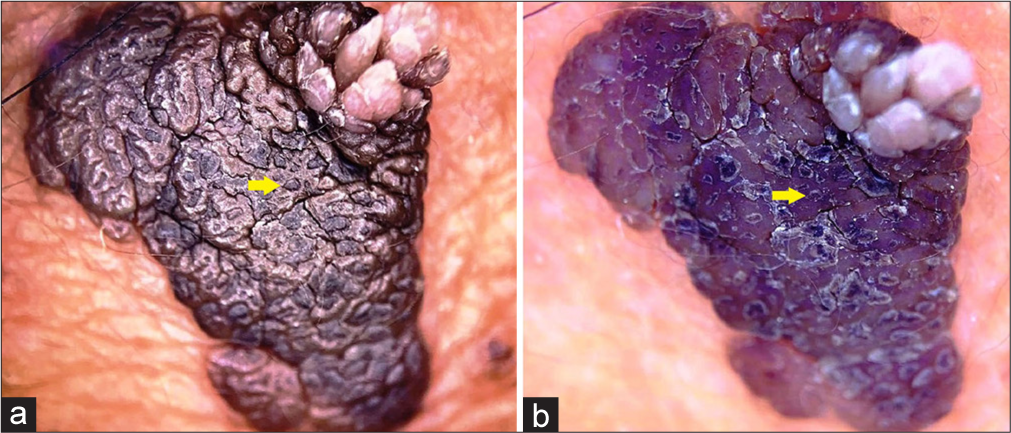
The colour imparted by a vascular lesion is primarily red due to the haemoglobin. Other colours that may be associated with a vascular lesion are bluish-black (deoxygenated haemoglobin/thrombosed vessel) and brown due to haemosiderin deposits in old lesions indicating a resolved haemorrhage [Figure 8].[3]
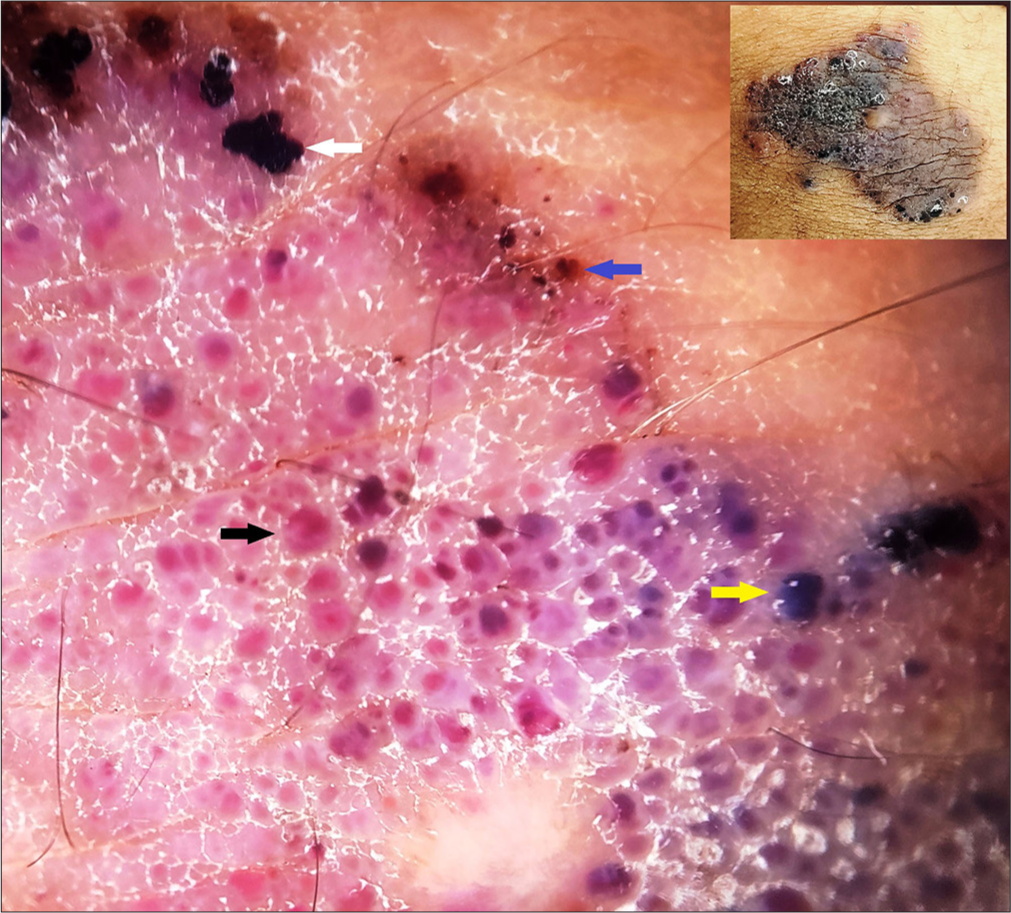
- Illustration of various colors of hemoglobin in a vascular malformation: red color of oxygenated hemoglobin (black arrow), black (white arrow) and purple (yellow arrow) colors of deoxygenated hemoglobin, and brown color of residual hemosiderin (blue arrow). Inset – clinical image.
18. c
Refer answer 12 and Figure 7.
19. c
Refer answer 12 and Figures 7 and 8.
20. b
Refer answer 12 and Figure 7.
21. c
Due to Tyndall effect, melanin at various levels in the dermis [Figure 7] appears as grey (papillary dermis), bluish-grey (upper reticular dermis), bluish (mid reticular dermis) and bluish-black (deep reticular dermis).[3]
22. b
In dermoscopic jargon, ‘pigmented lesion’ implies a melanocytic (lesions with melanocytic hyperplasia) and/or a melanotic (increased melanin without melanocytic hyperplasia) lesion.[9]
23. c
Although a pigmented lesion may depict all the patterns mentioned, pigmented lines forming reticular pattern [Figure 9] are prototypical. In the network pattern, the pigmented lines correspond to the melanin in the tips of the rete ridges and the ‘holes’ in between to the tips of the dermal papillae with relatively less melanisation.[10]
24. b

- A typical pigment network (brown lines in a reticulate pattern) seen in a non-facial pigmented lesion.
Dermoscopic findings are documented either using descriptive-analytical terminologies or metaphoric analogies or a combination of both. Table 1 outlines the comparison between both techniques. While metaphoric description is easier, a descriptive analysis should be the standard approach.[1]
| Descriptive analysis | Metaphoric analysis |
|---|---|
| Description of the features seen ‘as is’ | Pictorial analogy |
| Not influenced by variations in features | Variations in features may not match the analogy |
| Universally comprehendible | Subject to individuals’ perception/imagination, not universally comprehendible |
| Tedious and lengthy | Easier |
Example: Radial lines converging onto a common center |
Example: Spoke-wheel structure |
25. b
Refer answer 24.
Ethical approval:
Institutional Review Board approval is not required.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Basics of Dermoscopy In: Sacchidananda S, ed. IADVL Textbook of Dermatology (5th ed). Mumbai: Bhalani Publishing House; 2022. p. :187-94.
- [Google Scholar]
- Dermoscopy: An Overview of the Principles, Procedure and Practice In: Ankad BS, Mukherjee SS, Nikam BP, eds. Dermoscopy - Histopathology Correlation (1st ed). Singapore: Springer; 2021. p. :1-13.
- [CrossRef] [Google Scholar]
- A Kaleidoscopic Navigation through Different Shades of Colors in Dermoscopy. Nepal J Dermatol Venereol Leprol. 2024;22:3-10.
- [CrossRef] [Google Scholar]
- Polarized and nonpolarized dermoscopy: The explanation for the observed differences. Arch Dermatol. 2008;144:828-9.
- [CrossRef] [PubMed] [Google Scholar]
- Shiny White Structures. Available from: https://dermoscopedia.org/Shiny_white_structures [Last accessed on 2024 Sep 13]
- [Google Scholar]
- Dermoscopy of Penile Sclerosing Granuloma. BMJ Case Rep. 2021;14:e239846.
- [CrossRef] [PubMed] [Google Scholar]
- Pigmented Skin Lesions. Available from: https://dermnetnz.org/topics/pigmented-skin-lesions#:~:text=Pigmented%20skin%20lesions%20refer%2to,red%2C%20purple%20or%20blue) [Last accessed on 2014 Sep 13]
- [Google Scholar]
- Dermoscopic Pigment Network: Characteristics in Non-melanocytic Disorders. Indian Dermatol Online J. 2020;11:146-53.
- [CrossRef] [PubMed] [Google Scholar]






