Translate this page into:
Trichoteiromania Presenting as a Patch of Localised Hair Loss: A Diagnostic Challenge
*Corresponding author: Akash Agarwal, Department of Dermatology, Venereology, Leprosy, IMS and SUM Hospital, Bhubaneswar, Odisha, India. akash.22.1995@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Pramanik A, Panda M, Agarwal A. Trichoteiromania Presenting as a Patch of Localised Hair Loss: A Diagnostic Challenge. Indian J Postgrad Dermatol. 2025;3:86-7. doi: 10.25259/IJPGD_134_2024
Dear Editor,
A 29-year-old male, an engineer by profession, presented to the dermatology outpatient department with a localised patch of hair loss associated with intense pruritus over the scalp for 2 months. On examination, a well-defined mildly raised lichenoid plaque of size 1 × 0.5 cm was observed over the vertex. The overlying area showed short broken hairs of a maximum length of 0.5 cm with adherent whitish scales [Figure 1]. The rest of the scalp appeared normal. The hair pull test was negative. The patient denied pulling, cutting or eating scalp hair or application of any topical preparations. The patient also denied any tingling or burning sensation associated with the itch. There was no history of eczema, psoriasis, seborrheic dermatitis, alopecia or any significant medical history. A differential diagnosis of trichoteiromania, scalp dysesthesia, tinea capitis and trichotillomania with secondary lichen simplex chronicus was considered.

- Solitary well-defined lichenoid plaque over the vertex of the scalp.
A potassium hydroxide mount of the hair follicle and scales revealed no fungal elements. Trichoscopy performed with a dermlite-4™ dermoscope along with an iPhone X™ attachment (×10 magnification) under polarised mode revealed splitting of the hair shafts without proper delineation due to whitish scaling. On adding an interface liquid (liquid paraffin), it showed white structureless areas with few red dots (possibly blood crust secondary to repeated scratching) and monotonous clusters of broom hairs over the entire plaque [Figure 2]. A 4 mm punch biopsy from a representative site showed marked hyperkeratosis, hypergranulosis and acanthosis with regular elongation of rete ridges, vertically arranged collagen fibres with non-specific dermal infiltration and no hair-shaft deformity ruling out trichotillomania [Figure 3]. A psychiatry referral was given in view of suspected obsessive-compulsive disorder (OCD), which revealed that the repetitive itch was compulsive behaviour aggravated during stressful episodes related to his P.H.D thesis preparations.

- Trichoscopy (with interface liquid) (×10 magnification) shows white structureless areas (red circle) with red dots (blue arrows) and monotonous clusters of broom hairs (yellow arrows) over the entire plaque.
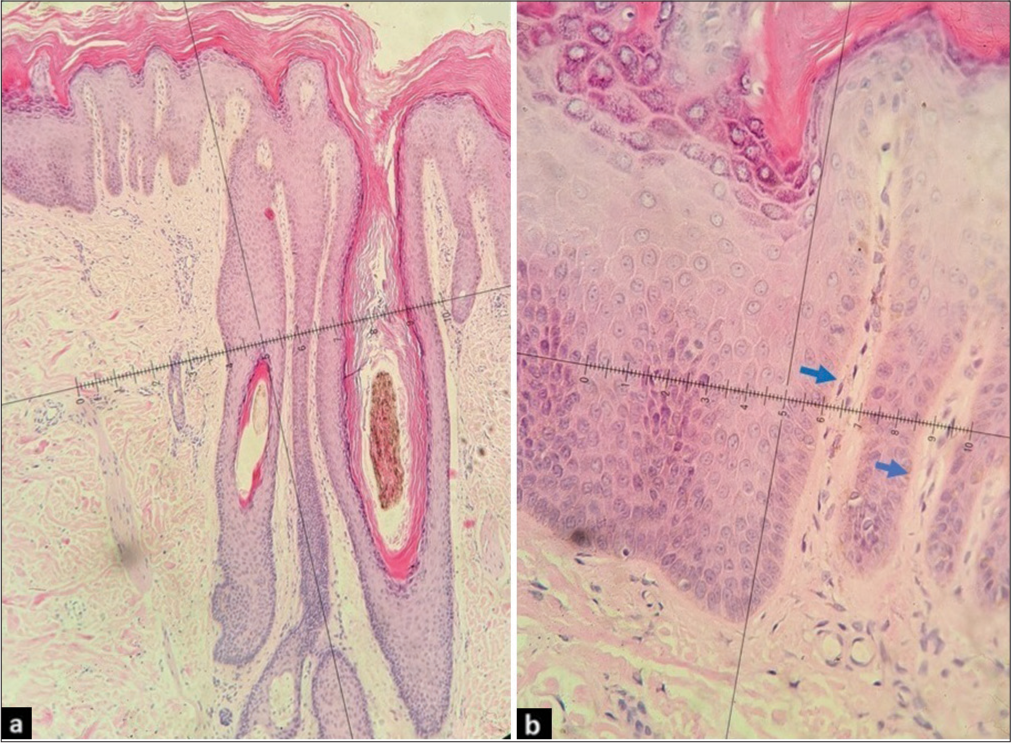
- (a) Haematoxylin and Eosin (H and E) (×10 magnification) – marked hyperkeratosis, hypergranulosis and acanthosis with regular elongation of rete ridges, no hair-shaft deformity. (b) H and E (×40 magnification) – vertically arranged collagen fibres (blue arrows) with non-specific dermal infiltration.
Based on the clinical, dermoscopic and histopathological examination, a final diagnosis of trichoteiromania was made. The patient was managed with tablet n-acetyl-cysteine, topical corticosteroids and anti-histamines. Behavioural strategies included habit reversal training and establishing activities to prevent rubbing. The patient responded well to therapy and is currently under regular follow-up.
The word trichoteiromania is derived from the Greek word ‘teiro’ which means ‘I rub’. It is a self-inflicted traumatic hair injury caused by repetitive rubbing of the scalp that subsequently causes fracturing of the hair shaft. Continuous scratching or rubbing can cause longitudinal splitting of the hair shafts into finer segments which give a brush or broom-like appearance. These monotonous broom hairs are a classical feature described in trichoteiromania of the scalp but are not specific.[1-3]
In our patient, many differentials were considered due to similar clinical morphology. Tinea capitis was ruled out based on potassium hydroxide mount and the absence of suggestive findings on trichoscopy and histopathology. Scalp dysesthesia, a variant of cutaneous dysesthesia syndrome, can also present with chronic itch over the scalp with secondary trichoteiromania and lichenoid changes. However, these patients often have a neurogenic cause and lack a component of OCD.[4] Trichotillomania was the closest differential but lack of typical trichoscopic findings such as the V sign, broken hair of uneven length, hook hair and flame hair along with histopathological findings of intact hair shaft ruled out its possibility.[5]
In such clinical scenarios, confusion always persists as to whether the itch was neurogenic or psychiatric which is what drives the management eventually. Monotonous broom hairs on trichoscopy should not be considered as diagnostic of trichoteiromania as other dermatoses also can show similar presentation. Hence, careful history-taking and psychiatric evaluation, along with dermoscopic and histopathological correlation is mandatory to reach an appropriate diagnosis.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Monotonous Broom Hairs: A Feature of Trichoteiromania. Skin Appendage Disord. 2020;6:168-70.
- [CrossRef] [Google Scholar]
- Videodermoscopy of Trichoteiromania: It is Beyond Broom Hairs. Indian Dermatol Online J. 2022;13:268-9.
- [CrossRef] [Google Scholar]
- Trichoteiromania: Good Response to Treatment with N-Acetylcysteine. Skin Appendage Disord. 2019;5:242-5.
- [CrossRef] [Google Scholar]
- Trichoscopic Diagnosis and Management of a Case of Scalp Dysesthesia with Lichen Simplex Chronicus. Int J Trichology. 2022;14:218-20.
- [CrossRef] [Google Scholar]
- Diagnostic Accuracy of Trichoscopy in Trichotillomania: A Systematic Review. Acta Derm Venereol. 2021;101:adv00565.
- [CrossRef] [Google Scholar]






