Translate this page into:
Mycetoma Due to Rare Fungus
*Corresponding author: Parag Suresh, Department of Dermatology, Vardhman Mahavir Medical College and Safdarjang Hospital, New Delhi, India. paragsuresh95@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kathuria S, Suresh P, Capoor MR. Mycetoma Due to Rare Fungus. Indian J Postgrad Dermatol. 2025;3:94-6. doi: 10.25259/IJPGD_142_2024
Dear Editor,
Eumycetoma is a chronic granulomatous infection characterised by subcutaneous swelling, discharging sinuses and grains caused by fungi. It is important to differentiate eumycetoma from actinomycetoma as management and treatment differ. For many years, surgical debridement and amputation were the only treatments for eumycetoma, but with the advent of newer antifungals, it has been possible to treat eumycetoma with medical therapy.[1] We discuss a case of mycetoma caused by Scedosporium apiospermum which responded very well to itraconazole.
A 50-year-old male presented with a plaque on left sole with multiple nodules and discharging sinuses for 2 years. The patient was apparently well 3 years back when he developed a nodule on left sole. Over a year, he developed multiple similar nodules and underlying swelling, which have been gradually increasing. Some nodules erupted to form sinuses discharging blood-stained discharge. There was no history of discharge of grains. Lesions were painless but swelling caused mild difficulty in walking. He reported a history of thorn prick 10 years back. There was no history of fever, weight loss, cough or systemic symptoms. The patient was empirically started on doxycycline and cotrimoxazole for 3 weeks with no improvement. On examination, there was an ill-defined 8 × 5cm hyperpigmented indurated swelling on left mid-sole. The swelling was studded with multiple nodules with haemorrhagic crusts of size 0.5 × 0.5 cm and discharging sinuses [Figure 1]. There was no significant lymphadenopathy.

- (a) Lesion at baseline. Multiple discharging sinuses on an indurated plaque. (b) Lesion after 4 months of itraconazole. (c) Lesion at 17 months (8 months after stopping itraconazole).
Direct microscopy using potassium hydroxide 10% showed fungal elements. Gram stain and acid fast bacilli smear did not reveal any organism. Culture of biopsied tissue revealed growth of Scedosporium spp. sensitive to ketoconazole and voriconazole [Figure 2]. Histopathology of nodule showed hyperkeratosis and parakeratosis with focal crusting. Underlying subepithelium showed acute on chronic inflammatory cells with numerous plasma cells, lymphocytes and neutrophils. No grains could be seen in deeper section. Sensitivity to itraconazole and amphotericin B was not done. Routine investigations including haemogram, liver and kidney function tests, blood sugar, urine and stool microscopy. Serology for human immunodeficiency virus, hepatitis B & C virus was non-reactive. Chest X-ray and ultrasound abdomen were within normal limits. Foot X-ray was normal but computed tomography (CT) scan of foot showed subcutaneous thickening without a bony lesion.
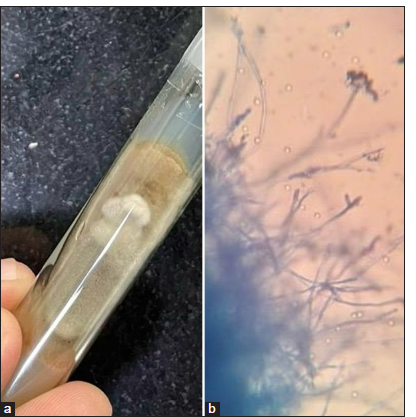
- (a) Scedosporium apiospermum growing as colonies with fluffy powdery texture with a light grey to brownish colour on Sabouraud’s dextrose agar. (b) Septate hyphae with slender and branching structures, some showing conidia at their tips.
Since voriconazole could not be afforded, the patient was started on itraconazole 200 mg twice daily. Within 4 months, there was significant improvement [Figure 1] and complete improvement after 6 months. The patient continued for 2 more months (total treatment 8 months) after complete resolution and then stopped himself as he contracted COVID-19. After 8 months of stopping treatment, there was no relapse [Figure 1].
Mycetoma has been labelled by the World Health Organization as a neglected tropical disease causing disability and morbidity.[1] The diagnosis is clinical based on discharging sinuses and extrusion of grains, but identifying its aetiological agent often poses lot of problems. S. apiospermum is an uncommon cause of pale-grain mycetoma. It belongs to group of hyalohyphomycosis characterised by the presence of hyaline hyphae, of which Scedosporium prolificans, Shigella boydii and S. apiospermum are the most common causes of human infections.[2] S. apiospermum is a soil saprophyte, known to cause cutaneous, subcutaneous, respiratory and disseminated infections in humans, both immunocompromised and immunocompetent.[2] It can present in various ways in skin such as pale-grain eumycetoma, abscess, lymphocutaneous syndrome, folliculitis, ulcers, plaques, nodules and other subcutaneous infections depending on mode of transmission and immune status of patient.[2,3] Other organisms causing pale grain eumycetoma include Fusarium spp., Acremonium falciforme and Aspergillus nidulans.
Histopathology is similar to other suppurative granulomatous conditions with neutrophils, neutrophilic debris surrounded by epithelioid cell granulomas. Often fungal hyphae can be well visualised in the centre of the granulomas on staining with periodic acid schiff or gomori methenamine silver (PAS or GMS) stains. Direct microscopy of the smears from the discharge in potassium hydroxide, Gram stain and modified Ziehl–Neelsen stain helps to delineate the bacterial or fungal aetiology of mycetoma. Wet dressing over the sinuses, skin biopsy and grains if seen are sent for culture. Common culture media used are Sabouraud’s dextrose agar or Potato dextrose agar with antibiotics and without cycloheximide. Radiological imaging such as ultrasound, CT scan or magnetic resonance imaging helps to identify the extent of involvement and to delineate bony involvement. Soft-tissue hypertrophy, osteolysis which is often irreversible and cavities (geodes) are all features of bony involvement.
Scedosporium species per se is resistant in vitro to most antifungals and azoles based regimens are superior to amphotericin B and 5-flucytosine, voriconazole being most effective and considered first-line drug, but cost is a limiting factor. In non-responsive cases, surgical debridement must be done and combination therapy of voriconazole and terbinafine is suggested.[2,3] Itraconazole is a cost-effective broad spectrum azole used widely in the treatment of eumycetoma.[1,3] In few case reports and series, combination of azoles with terbinafine, sequential therapy of azoles and terbinafine, caspofungin and miltefosine has been found useful. Our case responded very well to itraconazole 200 mg given twice daily and is currently under follow-up with no recurrence.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship:
Nil.
References
- WHO – Mycetoma. Available from: https://www.who.int/buruli/mycetoma/en [Last accessed on 2020 Apr 14]
- [Google Scholar]
- Scedosporium and Lomentospora An Updated Overview of Underrated Opportunists. Med Mycol. 2018;56(Suppl 1):102-25.
- [CrossRef] [PubMed] [Google Scholar]
- European Society of Clinical Microbiology and Infectious Diseases Fungal Infection Study Group; European Confederation of Medical Mycology. ESCMID and ECMM joint Guidelines on Diagnosis and Management of Hyalohyphomycosis: Fusarium spp., Scedosporium spp. and others. Clin Microbiol Infect. 2014;20(Suppl 3):27-46.
- [CrossRef] [PubMed] [Google Scholar]






