Translate this page into:
Evaluation of Efficacy and Safety of Fractional CO2 Laser Versus Micro-Needling with Autologous Platelet-Rich Plasma in Treatment of Acne Scars – A Split Face Study
*Corresponding author: Tanvi Mohit Patil, Department of Dermatology, MIMER Medical College, Pune, Maharashtra, India. dr.tanvipatil96@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Patil TM, Gokhale NR. Evaluation of Efficacy and Safety of Fractional CO2 Laser Versus Micro-Needling with Autologous Platelet-Rich Plasma in Treatment of Acne Scars – A Split Face Study. Indian J Postgrad Dermatol. 2025;3:13-8. doi: 10.25259/IJPGD_74_2024
Abstract
Objectives:
Acne and the resulting scars affect 90% of adolescents, posing a significant challenge for young adults. This study compares the efficacy and safety of two widely-used treatments: Fractional CO2 laser and micro-needling with platelet-rich plasma (PRP), to determine a cost-effective solution with comparable results.
Materials and Methods:
A hospital-based study was conducted at a dermatology outpatient department involving 60 participants. Goodman Barron scores were recorded for both sides of the face at baseline. One side received monthly treatments of Dermapen micro-needling with topical and intradermal PRP, while the other side was treated with fractional CO2 laser for 4 months (four sessions). Assessments were made at 4 and 6 months, and adverse effects were recorded.
Results:
Both treatments showed significant quantitative improvements after four sessions and at 6 months, with fractional CO2 laser achieving a 67% improvement and micro-needling with PRP achieving 65.2%. Subjective assessments indicated comparable outcomes (P > 0.05). Notably, laser treatment resulted in post-inflammatory hyperpigmentation in 10% of cases.
Conclusion:
Fractional CO2 laser and micro-needling with PRP demonstrate similar efficacy and safety in treating acne scars. Due to fewer side effects and quicker recovery observed with the combination therapy, it serves as a cost-effective alternative to fractional CO2 laser for acne scar treatment.
Keywords
Acne scars
Fractional CO2 laser
Goodman Barron score
Micro-needling
INTRODUCTION
Acne, a common and self-limiting inflammatory disorder of the pilosebaceous unit, usually affects adolescents and manifests as a variety of lesions including comedones, papules, pustules, nodules and cysts, which frequently result in facial scarring.[1] Severe acne often causes atrophic and hypertrophic scars, with ice pick, rolling and box scars being the most common.[2]
Dermatologists face major challenges while treating acne scars. Chemical peels, dermabrasion, subcision, fillers and punch procedures are among the treatments available, but the sector still requires more cost-effective ways that produce comparable outcomes.[3]
Ablative lasers, such as carbon dioxide and Erbium YAG, have shown potential in healing atrophic acne scars using the selective photothermolysis approach. However, their long recovery times and accompanying morbidities, including erythema, post-inflammatory hyperpigmentation, hypopigmentation and scarring, limit their widespread use.[4] Therefore, there is a need for innovative therapeutic modalities that offer enhanced efficacy, safety and minimal downtime. Ablative fractional resurfacing is a breakthrough technology that uses small treatment zones to encourage controlled wound healing. This approach spares surrounding tissue and enables for rapid epidermal regeneration with fewer adverse responses than typical ablative lasers.[5] Based on this premise, the ablative fractional CO2 laser has emerged as the gold standard for treating acne scars, noted for its safety and efficacy.[6]
Microneedling is a promising treatment for acne scars. This minimally invasive approach breaks down collagen bundles in the superficial dermis, stimulating collagen formation beneath the epidermis and improving scar appearance.[7,8]
Platelet-rich plasma (PRP) is rich in platelet-derived growth factors, with an ideal concentration exceeding 10 lakhs platelets/μL and an enrichment range of 300–700%. High levels of these growth factors make PRP beneficial for various dermatological applications, including enhanced graft survival in hair transplants, acne scar management, skin rejuvenation and other cosmetic procedures.[9] PRP’s growth hormones and cytokines, such as platelet-derived growth factor, transforming growth factor, vascular endothelial growth factor, insulin-like growth factor, epidermal growth factor and interleukin-1, stimulate protein synthesis, collagen production, endothelial migration, angiogenesis and skin regeneration, thereby reducing scars through collagen deposition.[9]
This study focuses on comparing the efficacy and safety of two leading modalities-fractional CO2 laser and micro-needling with autologous PRP (intradermal and topical)-for treating acne scars. We aim to provide valuable insights into selecting the most suitable therapeutic approach for addressing the significant issue of acne scarring.
MATERIALS AND METHODS
A hospital-based prospective analytical study was conducted at department of dermatology of a tertiary care hospital. Study was commenced after approval from the Institutional Ethical Committee. Study included a total of 60 cases after taking written informed consent.
Sampling type
This study was purposive sampling.
Sample size
Considering the study done by Rajput et al.,[10] the difference in baseline mean and standard deviation reported is 26.2 ± 6.31 and 26.8 ± 7.67 and using the formula:
Z = 1.96 at alpha =0.5
With 20% loss to follow-up, the minimum required sample size was 60 patients.
Inclusion criteria
Cases from all age groups and genders
Fitzpatrick skin types III–V
No history of previous treatments such as skin resurfacing procedures, chemical reconstruction of skin scars, microneedling, or laser therapy
An acne-free period of at least 6 months before recruitment.
Exclusion criteria
Pregnancy or breastfeeding
Use of photosensitising agents
Keloidal tendencies
Pacemaker implantation history
Cases unwilling to provide consent
Acne flare-ups during the study duration.
Participants were randomly assigned to receive fractional CO2 laser treatment on one side of the face and micro-needling plus PRP on the other side to ensure standardisation. The study employed a triple-blind design, where the participants, the dermatologists administering the treatments and the dermatologists assessing the outcomes were all blinded to the treatment assignments. Baseline Goodman Barron scores were recorded for both sides of the face. Treatments were conducted monthly for 4 months. Goodman Barron scores were re-evaluated at the end of the 4 months, followed by a 2-month remodelling period, with the final assessment at 6 months. Any adverse effects were documented.
Six months post-treatment, outcomes were evaluated by a second dermatologist, blinded to the treatment groups, using photographs of both procedures. Subjective grading was based on the following scale: Grade Four improvement (>75% improvement), Grade Three (51–75% improvement), Grade Two (26–50% improvement) and Grade One improvement (<25%).
Patients were asked to assess their results on a visual analogue scale of 0–10 at each session. Satisfaction scores for the right and left halves of each patient were recorded as follows: 0 for no response, 1–3 for poor response, 4–5 for fair response, 6–7 for good response and 8–10 for excellent response.
Group A: Fractional carbon dioxide laser
The Hironic MIXEL fractional CO2 10,600 nm laser (depth 895 μm) was used for the procedure. Before each session, eutectic mixture of local anesthetics (EMLA) cream (lidocaine 2.5% and prilocaine 2.5%) was applied to the target area for 40 min, followed by cleansing and disinfection with povidone iodine and 70% isopropyl alcohol. Eye shields protected the eyes. Based on our clinical experience, and guidelines from Jung et al. (2010),[11] we used high energy settings up to 60 mJ with a density of 100 mtz/cm2, primarily using a single pass to mitigate hyperpigmentation risk in Fitzpatrick skin types III–V. While this study provides a solid foundation, more recent guidelines, such as the 2022 International Consensus Recommendations by Salameh et al., suggest updated energy settings.[12] Subsequent sessions increased to 2–3 passes based on patient response. Cooling with ice packs for 5–10 min post-treatment and a pulse width of 0.5 mm provided effective and safe results. After treatment, the area was wiped with cold water, and patients were advised to apply sunscreen and emollients, avoiding sun exposure for 48 h. Any erythema was managed with topical steroids, and non-steroidal anti-inflammatory drugs were used for pain relief.
Group B: Micro-needling with PRP
Pre- and post-procedural protocols were identical for both groups. Micro-needling was performed using a dermapen at a depth of 2 mm during the first session, which was increased to 3 mm based on patient tolerability and response. The skin was stretched in vertical, horizontal and diagonal directions, with minimal pressure applied until uniform bleeding points appeared over the scarred area. Moist gauze was used for haemostasis.
PRP was prepared using the double-spin method. The PRP preparation technique followed in this study was based on the method described by Asif et al. in their study on PRP and micro-needling.[9] A 20-mL syringe containing 3 mL of anticoagulant and 17 mL of blood was used. After a 5-min soft spin, the plasma and buffy coat were extracted. A 2nd 17-min hard spin separated the platelet-rich zone from platelet-poor plasma (PPP). Two mL of PPP were removed, leaving PRP. For acne scars, 1 mL of PRP was injected intradermally at 0.1 mL/cm2, and the remaining 1 mL was applied topically.
Data analysis
Data were noted down in a pre-designed study pro forma. Analysis of Goodman Barron scores between both the groups was done using Mann–Whitney Test between the groups and with Wilcoxon sign-rank test within the groups. P < 0.05 was taken as level of significance. The Statistical Package for the Social Sciences Version 26.0 was used for data analysis.
RESULTS
The average age of the participants was 22.91 years, with half of the cases falling between 21 and 25 years old. The study included 76.7% females and 23.3% males. The Goodman Barron scores for both sides of the face were comparable at baseline. Post-treatment, both groups showed significant improvements in quantitative scores after four sessions, which further improved by the 6-month mark. At baseline, the score was 18.2 for Group A compared to 17.8 for Group B. In Group A, the score significantly reduced to 7.4 by the end of 4 months and further reduced to 6.0 by 6 months (P < 0.001 and P = 0.014), reflecting an improvement of 59.3% and 67.0%, respectively. In Group B, the score significantly reduced to 7.6 by the end of 4 months and further reduced to 6.2 by 6 months (P < 0.001 and P = 0.021), reflecting an improvement of 57.3% and 65.2%, respectively. There was no statistically significant difference between the study groups (P > 0.05) [Table 1 and Figure 1].
| Goodman and Baron score | Group | P-value | |||
|---|---|---|---|---|---|
| A | B | ||||
| Mean ± SD | Age improvement (%) | Mean ± SD | Age improvement (%) | ||
| Baseline | 18.2±2.71 | 17.8±1.76 | 0.57 | ||
| 4 months* | 7.4±0.91 | 59.3 | 7.6±1.08 | 57.3 | 0.39 |
| 6 months* | 6.0±0.78 | 67.0 | 6.2±1.01 | 65.2 | 0.44 |
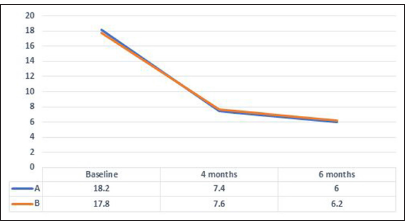
- Change in Goodman and Baron in both groups. Blue color indicates Group A = CO2 Laser, Orange color indicates Group B = Microneedling and PRP. PRP: Platelet-rich plasma.
Subjective assessments by a blinded observer indicated that grade IV improvement (>75%) was observed in 16.7% of cases in Group A and 10% in Group B. Grade III (51–75%) and Grade II (26–50%) improvements were observed in 45% and 38.3% in Group A, and 43.3% and 46.7% in Group B, respectively. Subjective assessments also indicated comparable improvement between the groups (P = 0.47) [Table 2].
| Subjective assessment | Group* | |
|---|---|---|
| A | B | |
| Grade 1 | 0 | 0 |
| 0.0% | 0.0% | |
| Grade 2 | 23 | 28 |
| 38.3% | 46.7% | |
| Grade 3 | 27 | 26 |
| 45.0% | 43.3% | |
| Grade 4 | 10 | 6 |
| 16.7% | 10.0% | |
| Total | 60 | 60 |
| 100.0% | 100.0% | |
*P value - 0.47 (No significant difference between both groups)
Patient satisfaction scores revealed that the right half of the face had excellent responses in 8 patients, good responses in 31 patients, fair responses in 20 patients and poor responses in one patient. The left half of the face had excellent responses in four patients, good responses in 28 patients, fair responses in 27 patients and poor responses in one patient [Figure 2].
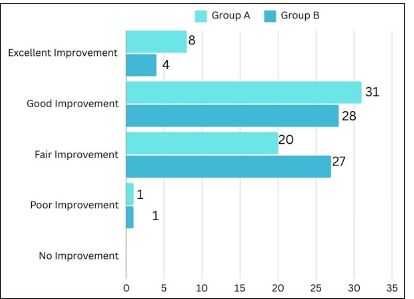
- Final patient satisfaction scores.
Minor adverse events were noted in both groups, such as erythema (5% in Group A and 1.7% in Group B), burning sensation (10% in Group A and 8.3% in Group B), pain (3.3% in Group A and 1.7% in Group B) and bruising (1.7% in Group A). The only significant adverse effect observed with laser treatment was post-inflammatory hyperpigmentation (10% in Group A vs. 1.7% in Group B) [Table 3].
| Adverse drug reactions | Group | P-value | |
|---|---|---|---|
| A (%) | B (%) | ||
| Erythema | 3 (5) | 1 (1.7) | 0.61 |
| Burning sensation | 6 (10) | 5 (8.3) | 1.00 |
| Hyperpigmentation | 6 (10) | 1 (1.7) | 0.03 |
| Pain | 2 (3.3) | 1 (1.7) | 1.00 |
| Bruising | 1 (1.7) | 0 | 1.00 |
Group A: CO2 Laser
Case 1.
Pre-treatment score – 24 and post-treatment score – 11 [Figure 3].
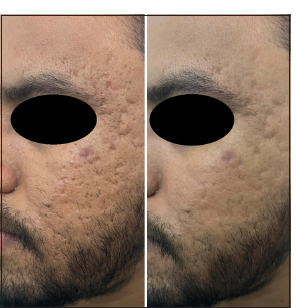
- Pre-treatment score – 24 and Post treatment score – 11.
Group B: Microneedling and PRP
Case 1.
Pre-treatment score – 20 and post-treatment score – 9 [Figure 4].

- Pre-treatment score – 20 and Post treatment score – 9.
DISCUSSION
The study’s participants averaged 22.91 years, with 50% aged 21–25, aligning with findings by Abdel Kareem et al., Majid and Imran and Anupama and Wahab.[13-15] A female predominance, consistent with Apfelberg et al., was noted.[16] Both fractional CO2 laser and micro-needling plus PRP treatments showed significant improvements after four sessions, with further enhancements at 6 months.
The study’s results align with Pooja et al., showing improvement rates of 47.1% and 68.7% for fractional CO2 laser, 41.9% and 60.3% for micro-needling and 13.6% and 31.1% PRP after 2nd and 4th sitting, respectively. Maximum improvement in rolling scars was seen with microneedling (62%) followed by CO2 laser (57%) whereas better improvement in boxcar scars was seen with CO2 laser (66%) followed by microneedling (54%).[17] Rajput et al. also found both treatments equally effective for acne scars.[10]
Our study’s qualitative results mirrored those observed by Pooja et al., with fractional CO2 laser generally outperforming micro-needling based on subjective assessments. However, the difference in subjective assessments between the two groups was not statistically significant.[17]
Both groups experienced minor adverse events such as erythema, burning sensation, pain and bruising. The only significant adverse effect observed with the laser treatment was post-inflammatory hyperpigmentation (10% vs. 1.7%). These findings are consistent with those reported by Rajput et al. and Pooja et al., both of whom noted post-inflammatory hyperpigmentation in the laser group.[10,17] This consistency in adverse event profiles underscores the safety and tolerability of both treatment modalities.
In summary, our study, when compared with existing literature, adds substantial value to the management of acne scars. The comparable efficacy and safety of fractional CO2 laser and combining micro-needling with PRP provide viable treatment options, allowing clinicians to tailor treatments based on individual patient needs and preferences.
Prevalent knowledge
Fractional CO2 laser, PRP and microneedling are established treatments, with fractional lasers having higher side effect rates while microneedling and PRP offer better safety profiles but may have lower efficacy.
New knowledge
Limited research exists on the combination of microneedling and PRP and its comparison with CO2 laser. Our study reveals that this combination provides comparable results with an improved safety profile.
Limitations
The lack of scar-type stratification limits generalizability, and the split-face design complicates attributing patient satisfaction exclusively to either treatment modality, introducing interpretive challenges. The single-centre design and subjective assessments may also introduce regional and inherent biases.
CONCLUSION
Our study demonstrates the significant efficacy of both fractional CO2 laser and micro-needling with autologous PRP in treating acne scars, showing comparable effectiveness 6 months post-treatment. Micro-needling with PRP is associated with fewer instances of hyperpigmentation and presents a cost-effective alternative to fractional CO2 laser, particularly in resource-limited settings. These findings support the integration of micro-needling with PRP as a safe and budget-friendly option for acne scar treatment. Further research is needed to standardise PRP preparation methods, including platelet counts and treatment responses, to optimize its use in clinical practice.
Ethical approval
The research/study approved by the Institutional Review Board at MIMER Medical College, Talegaon, number IEC/MIMER/2023/INST/864, dated 16 February 2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Effective Treatments of Atrophic Acne Scars. J Clin Aesthet Dermatol. 2015;8:33-40.
- [Google Scholar]
- Treatment of Acne Scarring with Fractional CO2 Laser. J Cosmet Laser Ther. 2012;14:162-5.
- [CrossRef] [PubMed] [Google Scholar]
- Fractional CO2 Laser Resurfacing for Atrophic Acne Scars: A Randomized Controlled Trial with Blinded Response Evaluation. Lasers Surg Med. 2012;44:447-52.
- [CrossRef] [PubMed] [Google Scholar]
- A New Modality for Fractional CO2 Laser Resurfacing for Acne Scars in Asians. Lasers Med Sci. 2013;28:627-32.
- [CrossRef] [PubMed] [Google Scholar]
- Acne Scarring Treatment Using Skin Needling. Clin Exp Dermatol. 2009;34:874-9.
- [CrossRef] [PubMed] [Google Scholar]
- Subcutaneous Incisionless (Subcision) Surgery for the Correction of Depressed Scars and Wrinkles. Dermatol Surg. 1995;21:543-9.
- [CrossRef] [PubMed] [Google Scholar]
- Combined Autologous Platelet-rich Plasma with Microneedling Verses Microneedling with Distilled Water in the Treatment of Atrophic Acne Scars: A Concurrent Split-face Study. J Cosmet Dermatol. 2016;15:434-43.
- [CrossRef] [PubMed] [Google Scholar]
- A Prospective, Nonrandomized, Open-label Study, Comparing the Efficacy, Safety, and Tolerability of Fractional CO2 Laser versus Fractional Microneedling Radio Frequency in Acne Scars. J Cutan Aesthet Surg. 2021;14:177-83.
- [CrossRef] [PubMed] [Google Scholar]
- Lower-fluence, Higher-density Versus Higher-fluence, Lower-density Treatment with a 10,600-nm Carbon Dioxide Fractional Laser System: A Split-face, Evaluator-blinded Study. Dermatol Surg. 2010;36:2022-9.
- [CrossRef] [PubMed] [Google Scholar]
- Energy-based Devices for the Treatment of Acne Scars: 2022 International Consensus Recommendations. Lasers Surg Med. 2022;54:10-26.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness of Subcision Using Carboxytherapy Plus Fractional Carbon Dioxide Laser Resurfacing in the Treatment of Atrophic Acne Scars: Comparative Split Face Study. J Dermatolog Treat. 2020;31:296-9.
- [CrossRef] [PubMed] [Google Scholar]
- Fractional CO2 Laser Resurfacing as Monotherapy in the Treatment of Atrophic Facial Acne Scars. J Cutan Aesthet Surg. 2014;7:87-92.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness of CO2 Laser with Subcision in Patients with Acne Scars. J Cosmet Laser Ther. 2016;18:367-71.
- [CrossRef] [PubMed] [Google Scholar]
- The Ultrapulse Carbon Dioxide Laser with Computer Pattern Generator Automatic Scanner for Facial Cosmetic Surgery and Resurfacing. Ann Plast Surg. 1996;36:522-9.
- [CrossRef] [PubMed] [Google Scholar]
- A Randomized Study to Evaluate the Efficacy Fractional CO2 Laser, Microneedling and Platelet Rich Plasma in Post-Acne Scarring. Indian Dermatol Online J. 2020;11:349-54.
- [CrossRef] [PubMed] [Google Scholar]







