Translate this page into:
Apocrine Hidrocystoma: A Candelabrum of the Eye – A Case Report
*Corresponding author: Shrinivas Patil, Department of Dermatology, Venereology and Leprosy, Command Hospital Air Force, Bengaluru, Karnataka, India. shrinivas93doctor@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Patil S, Iswariya J, Bhatnagar A, Mitra D, Mehta R. Apocrine Hidrocystoma: A Candelabrum of the Eye – A Case Report. Indian J Postgrad Dermatol. 2024;2:107-9. doi: 10.25259/IJPGD_12_2024
Abstract
Hidrocystomas are apocrine gland proliferations of the skin that are fluid filled and benign in nature. Two main types are recognised, namely apocrine and eccrine hidrocystoma, identified based on histological findings. Surgical excision is the treatment of choice, although various other modalities exist with varying success rates. We report a case of apocrine hidrocystoma, which is uncommonly reported, for which surgical excision gave good clinical and cosmetic outcomes.
Keywords
Apocrine hidrocystoma
Eccrine hidrocystoma
Benign
Surgical excision
Case report
INTRODUCTION
Hidrocystomas are apocrine gland proliferations of the skin that are fluid filled and benign in nature. There are two main types: apocrine and eccrine hidrocystomas, which are identified based on histological findings. Hidrocystoma resembles basal cell carcinoma, blue nevi, cutaneous melanoma, eccrine cystadenoma, follicular cyst, milia and syringoma, which need to be excluded by appropriate investigations. Due to the benign nature of the disease, surgical excision with narrow margins is the most usual treatment for apocrine hidrocystoma; however, a few other treatment modalities with varying success rates have been reported.
CASE REPORT
A 44-year-old male presented with solitary round raised, asymptomatic swelling over the inner aspect of the left eye for 3 years. The lesion was insidious in onset and gradually progressed in size without any discharge, redness or pain. There was no history of eye irritation, foreign body sensation and an inability to see. There was also no history of previous orbital trauma. On examination, there was a solitary dome-shaped papule measuring 80 × 70 mm over the medial canthus region of the left eye [Figure 1]. Palpation revealed the lesion to be non-tender, cystic in consistency and mobile. The ocular examination was otherwise within normal limits in both eyes. Dermoscopy was not done in our case which otherwise displays a translucent structure with a bluish hue, occasionally containing yellowish or brownish pigmentation. The cystic lesions may exhibit a central pore or punctum, surrounded by vascular structures such as linear or arborising vessels. These features aid in differentiation from other cystic lesions.[1] A shave biopsy of the lesion was performed under local anaesthesia. Histopathological evaluation revealed cystic spaces lined by inner columnar cells with surrounding dense fibro collagenous tissue. Immunohistochemistry revealed positive P63 and SMA; Her2 Neu was negative [Figure 2].

- (a and b) shows anterior and lateral view photographs showing solitary dome-shaped papule over medial canthus region of the left eye.
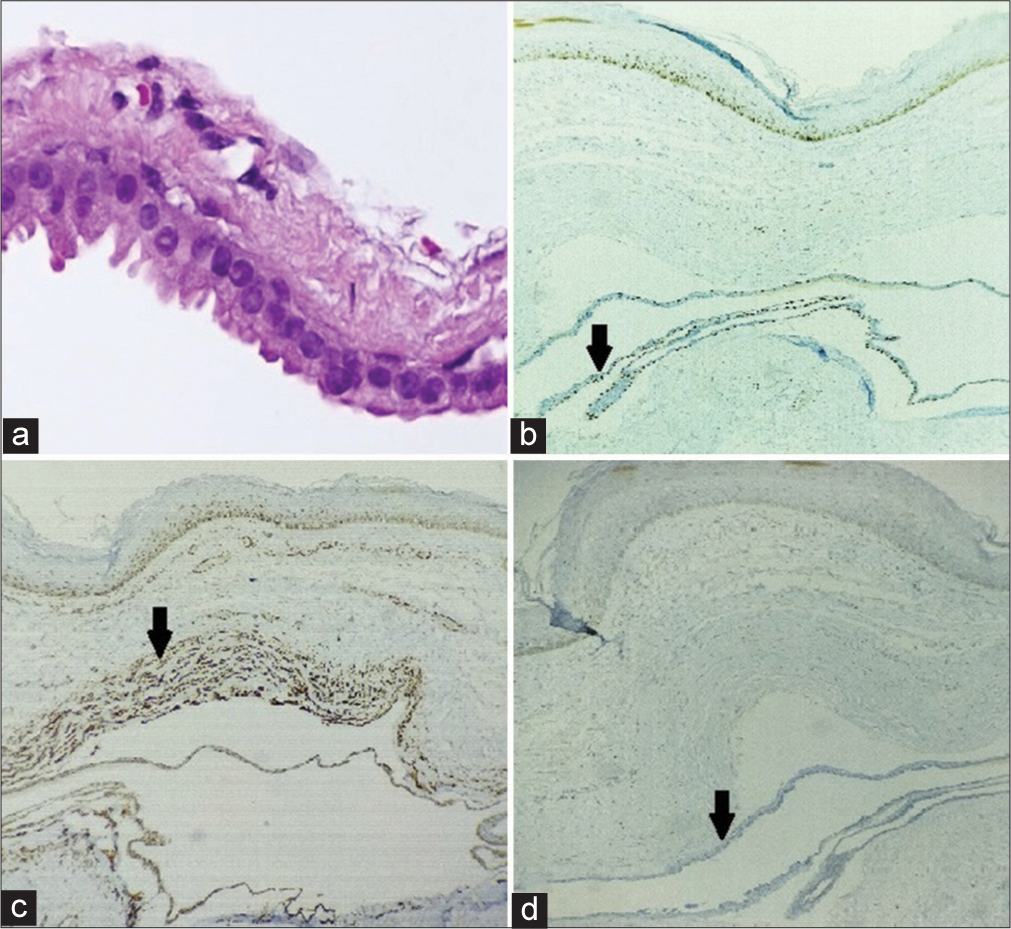
- (a) Histopathological examination (100x) shows inner layer of columnar cells, Immunohistochemical staining shows (b) p63 positive (black arrow), (c) Smooth muscle actin positive (black arrow), (d) Her2neu negative (black arrow).
DISCUSSION
Apocrine gland proliferations of the skin that are fluid filled and benign are known as hidrocystomas. Apocrine and eccrine hidrocystomas are identified based on histological findings. Cysts with several locations and apocrine secretion are known as apocrine hidrocystomas. A cystic tumour without decapitation secretion is less likely to be represented by eccrine hidrocystomas than by unilocular sweat retention in a dilatation duct or gland. Hidrocystomas typically manifest as solitary, soft, dome-shaped, translucent papules or nodules during adulthood. Primarily on the eyelids, particularly the inner canthus, they are sporadically present elsewhere, including the neck, trunk, penis, axillae and anal area. Differential diagnosis includes basal cell carcinoma, blue nevi, cutaneous melanoma, eccrine cystadenoma, follicular cyst, milia and syringoma. The recommended course of action for isolated lesions has always been surgical excision.[2] Due to the benign nature of the disease, surgical excision with narrow margins is the most usual treatment for apocrine hidrocystoma. This is the sole method that enables a medical professional to treat these tumours as well as make the final diagnosis. Needle piercing is an alternate treatment option, but it is often associated with local recurrence.[3] Eyelid apocrine hidrocystoma has been successfully treated with cyst puncture and hypertonic glucose sclerotherapy.[4] Another option for surgery is to use a trichloroacetic acid injection followed by aspiration after a cyst puncture.[5] In addition, botulinum toxin A[5] has been utilised with success.
CONCLUSION
The case underscores the importance of distinguishing hidrocystomas from other similar-appearing lesions such as basal cell carcinoma, blue nevi, cutaneous melanoma, eccrine cystadenoma, follicular cyst, milia, and syringoma through appropriate diagnostic investigations. Timely and accurate diagnosis followed by proper surgical intervention can ensure excellent clinical and cosmetic outcomes for patients with apocrine hidrocystomas.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Dermoscopy of Apocrine Hidrocystomas: A Morphological Study. Dermatology. 2014;228:153-8.
- [Google Scholar]
- Apocrine and Eccrine Hidrocystomas: A Clinicopathological Study. Acta Dermatovenerol Alp Pannonica Adriat. 2021;30:53-6.
- [CrossRef] [PubMed] [Google Scholar]
- Eccrine Hidrocystoma in a Child: An Atypical Presentation. Ann Dermatol. 2010;22:69-72.
- [CrossRef] [PubMed] [Google Scholar]
- A Minimally Invasive Approach for Apocrine Hidrocystomas of the Eyelid. Dermatol Surg. 2016;42:134-6.
- [CrossRef] [PubMed] [Google Scholar]
- Multiple Apocrine Hidrocystomas. Dermatol Online J. 2008;14:12.
- [CrossRef] [PubMed] [Google Scholar]







