Translate this page into:
Primary Cutaneous T-cell Lymphoma – A Diagnostic Dilemma
*Corresponding author: Kafil Akhtar, Department of Pathology, Jawaharlal Nehru Medical College, Aligarh, Uttar Pradesh, India. drkafilakhtar@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Usman SI, Adil M, Kratee K, Akhtar K. Primary Cutaneous T-cell Lymphoma – A Diagnostic Dilemma. Indian J Postgrad Dermatol. doi: 10.25259/IJPGD_148_2024
Abstract
Cutaneous lymphomas are a heterogenous group of neoplasm confined to skin at the time of diagnosis. These are extranodal non-Hodgkin lymphomas (NHLs). Here, we present a case of 58 years male who presented to the dermatology outpatient department with complaints of multiple painless nodules with petechial rashes over both arms, hand, trunk, body and legs, which were not associated with any other symptoms. A biopsy from one of the lesions was sent with clinical suspicion of sarcoidosis, pseudolymphoma and metastasis. On microscopic examination, diffuse infiltration of atypical cells in the dermis was seen with membranous positivity for CD45, CD3 and CD5. Based on the history, clinical examination and histopathological evaluation, a final diagnosis of T-cell NHL was given. Our patient was started on 6 cycles of 10 mg/m2 of doxorubicin and 50 mg/m2 of methotrexate per week. He is asymptomatic on 3 months of follow-up, with no new lesions and bearable side effects of chemotherapeutic agents.
Keywords
Cutaneous lymphoma
Immunohistochemistry
Pseudolymphoma
T-cell non-Hodgkin lymphoma NHL
INTRODUCTION
Primary cutaneous lymphomas are a heterogenous group of neoplasms, which are usually T-cell non-Hodgkin lymphoma (NHL) in contrast to nodal NHL which is predominantly B-cell types. Among T-cell cutaneous NHL, majority can be classified as mycosis fungoides (MFs) or Sezary syndrome.[1] Incidence of cutaneous T-cell lymphoma (CTCL) is showing a rising trend and more among African Americans.[2] CTCL predominantly affects males in the fifth decade of life. Poor prognosis is indicated by advanced disease stage, male sex, raised lactate dehydrogenase levels and large-cell transformation while hypopigmented and poikilodermatous MFs have a good prognosis.[3] Nearly, half of cutaneous lymphomas are MF, which occur slowly over years, progressing from macules to plaques to skin tumours or nodal involvement. On the other hand, Sezary syndrome is the aggressive form, characterised by pruritic erythroderma, generalised lymphadenopathy and atypical circulating large mononuclear cells with convoluted nuclei (Sézary cells).[4] Patients with CTCL also have more risk of secondary cancers such as melanoma, other NHL, breast and lung cancer and a proper evaluation should be done.[5] In particular, small cell carcinoma lung and NHL of other sites should always be evaluated during follow-up of patients of CTCL.[6]
CASE REPORT
A 58 years male presented to dermatology outpatient department with complaints of nodular eruptions with petechial rashes over dorsum of both hand and arms for the past 2 months, with a history of similar eruptions on the legs and trunk for the last fortnight. There is a history of similar numerous small red spots over the extremities and upper back since the past 10 years. These lesions were not associated with pain, discharge or itching. There was no history of any treatment or radiation exposure. There was history of low-grade fever off and on for 2 years. On examination, multiple hard, black to brown patches and nodules ranging from 1 cm to 4 cm were present over dorsum of both hands [Figure 1], arms and trunk. Poikilodermatous skin was seen in upper back.

- Clinical image showing petechial rashes and nodules on the dorsum of both hands.
Punch biopsy was sent for histopathologoic study to rule out differentials of sarcoidosis, cutnaeous metastasis and lymphoma. On microscopic examination, diffuse infiltration of dermis by intermediate to large atypical cells was seen. These cells had hyperchromatic nucleus with irregular nuclear membrane and scant eosinophilic cytoplasm [Figure 2]. The tumour cells were seen reaching up to the epidermis. To limit the differential diagnosis, immunohistochemistry was performed. The cells turned out to be clonal in nature with CD45, CD5 [Figure 3a] and CD3 [Figure 3b] positivity and negative for CD23 and CD19. Further, these cells were negative for p40 and HMB45, so any metastatic epithelial malignancy and melanoma were ruled out. A final diagnosis of T-cell cutaneous lymphoma was made. Our patient was started on six cycles of 10 mg/m2 of doxorubicin and 50 mg/m2 of methotrexate per week. He is doing fine on 3 months of follow-up, with no new lesions and bearable side effects of chemotherapeutic agents.
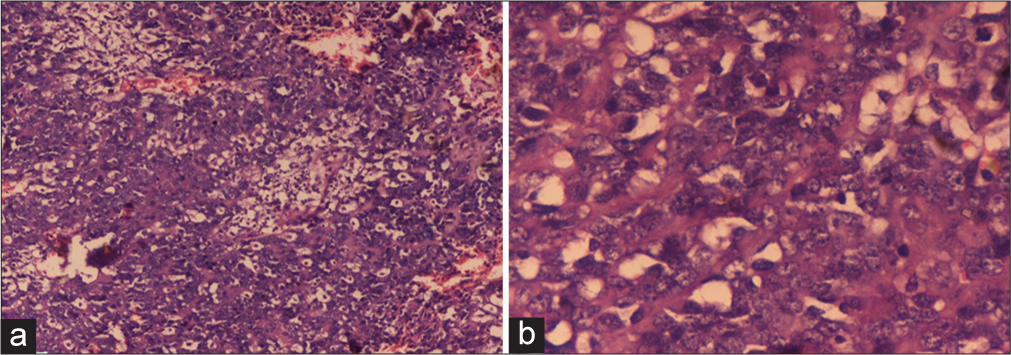
- (a) Section shows diffuse infiltration of dermis by intermediate to large atypical cells reaching up to the epidermis. Haematoxylin and Eosin ×10. (b) Section shows diffuse infiltration of dermis by intermediate to large atypical cells with hyperchromatic nucleus, irregular nuclear membrane and scant eosinophilic cytoplasm. Haematoxylin and eosin ×40.
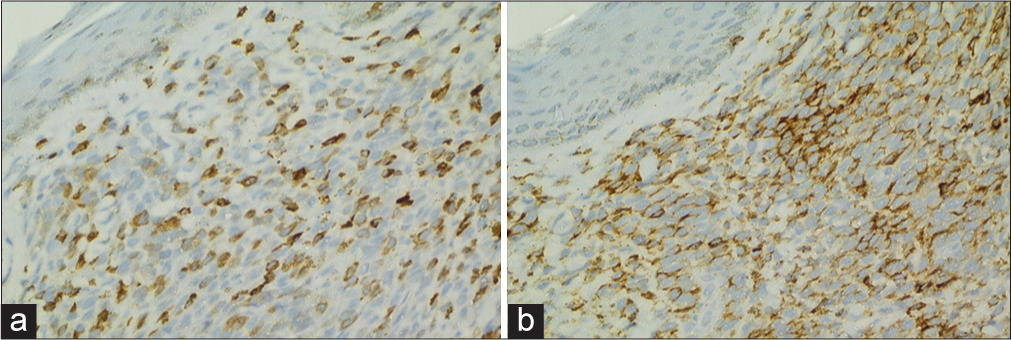
- (a) Immunohistochemistry showed positivity of tumour cells for CD5. Immunohistochemistry (IHC) CD5 ×40. (b) Immunohistochemistry showed positivity of tumour cells for CD3. IHC CD3 ×40.
DISCUSSION
Lymphoid infiltration of skin can be seen in both beingn as well as malignant conditions. Pseudolymphomas are the inflammatory conditions which mimic lymphoma on histopathology.[7] Since clinical features are overlapping, histopathological and immunohistochemical correlation is important to reach a final diagnosis. Psudolymphoma can display either a superficial band-like pattern, characterised by a dense superficial lymphocytic infiltration or a nodular/diffuse pattern, typified by dense, dermal diffuse or nodular infiltrates that extend into the subcutis without any epidermotropism. T-cell lymphoma (CTCL) is characterised by the presence of medium to large atypical lymphocytes with high proliferative index, epidermotropism, Pautrier’s micro-abscesses and lymphocyte tagging. Establishment of clonality by immunohistochemistry is of paramount importance.[8] Sometimes pseudolymphoma can transform into lymphoma, which presents as increase size of the lesion and atypia on microscopicy such as nuclear enlargement. However, it is still a matter of concern that whether it is transformation or previously misdiagnosed lymphoma.[9] In our case, there was diffuse infiltration of atypical cells and monoclonality, so the diagnosis of lymphoma was made. Since there was no other mass lesion seen on positron emission tomography-computed tomography and no granuloma seen on microscopic examination, other differentials of secondaries and sarcoidosis were ruled out.
Many management options are available for cutaneous lymphomas. Chemotherapeutic agents include bexarotene, methotrexate, vorinostat, belinostat, romidepsin, doxorubicin and gemcitabine. Current biological agents include Magrolimab, which is anti CD47, especially targeted in MF and Sezary syndrome.[10] The main aim of the treatment is to reduce the symptoms and prevent progression, with skin-directed therapies being the first line of treatment, followed by systemic therapies.[11] Important things to consider for treatment are the patient’s age, co-morbidities, and the extent of symptoms.[12] Our patient was started on six cycles of 10 mg/m2 of doxorubicin and 50 mg/m2 of methotrexate per week. He has no new lesions and has tolerable side effects of chemotherapy till a three months follow up.
CONCLUSION
Most CTCLs grow very slowly and are not life-threatening. The diagnosis of CTCLs is difficult at early stages because of the presence of variable clinical presentations and lack of definitive diagnostic criteria. But a strong clinical suspicion with skin changes and immunophenotyping goes a long way in the diagnosis.
Ethical approval:
Institutional Review Board approval is not required.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Cutaneous T-cell Lymphomas: 2023 Update on Diagnosis, Risk-stratification, and Management. Am J Hematol. 2023;98:193-209.
- [CrossRef] [Google Scholar]
- Incidence of Cutaneous T-cell Lymphoma in the United States, 1973-2002. Arch Dermatol. 2007;143:854-9.
- [CrossRef] [PubMed] [Google Scholar]
- Survival Outcomes and Prognostic Factors in Mycosis Fungoides/Sezary Syndrome: Validation of the Revised International Society for Cutaneous Lymphomas/European Organisation for Research and Treatment of Cancer Staging Proposal. J Clin Oncol. 2010;28:4730-9.
- [CrossRef] [PubMed] [Google Scholar]
- Genetics Abnormalities with Clinical Impact in Primary Cutaneous Lymphomas. Cancer (Basel). 2022;14:4972-3.
- [CrossRef] [PubMed] [Google Scholar]
- The Incidence of Other Primary Cancers in Patients with Cutaneous Lymphoma. Ann Dermatol. 2018;30:335-41.
- [CrossRef] [PubMed] [Google Scholar]
- Increased Risk of Secondary Cancers in Patients with Primary Cutaneous T Cell Lymphoma. J Invest Dermatol. 2000;115:62-5.
- [CrossRef] [PubMed] [Google Scholar]
- Approach to Cutaneous Lymphoid Infiltrates: When to Consider Lymphoma? Indian J Dermatol. 2016;61:351-74.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and Dermoscopic Features of a Case of Idiopathic T-Cell Pseudolymphoma. Indian Dermatol Online J. 2021;12:583-6.
- [CrossRef] [PubMed] [Google Scholar]
- Progression of Cutaneous B-cell Pseudolymphoma to Cutaneous B-cell Lymphoma. J Cutan Med Surg. 2002;6:519-28.
- [CrossRef] [PubMed] [Google Scholar]
- Targeting the CD47-SIRPα Axis: Present Therapies and the Future for Cutaneous T-cell Lymphoma. Cell. 2022;11:3591-2.
- [CrossRef] [PubMed] [Google Scholar]
- The Changing Therapeutic Landscape, Burden of Disease, and Unmet Needs in Patients with Cutaneous T-cell Lymphoma. Br J Haematol. 2021;192:683-96.
- [CrossRef] [PubMed] [Google Scholar]
- Primary Cutaneous T-cell Lymphoma (Mycosis Fungoides and Sézary Syndrome): Part II. Prognosis, Management, and Future Directions. J Am Acad Dermatol. 2014;70:1-17.
- [CrossRef] [PubMed] [Google Scholar]








