Translate this page into:
Innocence in Disguise: Vulvar Hidradenoma Papilliferum
*Corresponding author: Ankita Siddharth Shah, Department of Dermatology, Venereology and Leprosy, Deenanath Mangeshkar Hospital and Research Center, Pune, Maharashtra, India. ankita.phade95@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shah AS, Sadhwani M, Bhide DS, Kulkarni V, Vaidya PP, Patki AH. Innocence in Disguise: Vulvar Hidradenoma Papilliferum. Indian J Postgrad Dermatol. 2025;3:52-5. doi: 10.25259/IJPGD_224_2024
Abstract
The vulvar region contains a high concentration of apocrine, eccrine, anogenital mammary-like glands and pilosebaceous units. Vulvar hidradenomas are benign tumours originating from anogenital mammary-like glands and typically manifest as small, painless nodules on the vulva. They can clinically resemble pyogenic granulomas or granuloma inguinale. The preferred treatment method is local surgical excision. This case report discusses two cases of women diagnosed with vulvar hidradenomas, highlighting their characteristic clinical presentation and management approach. These cases serve as a reminder for clinicians to consider this rare tumour in differential diagnoses of nodular lesion on vulva with beefy red erosive surface, alongside conditions such as sexually transmitted infections and other benign or malignant tumours.
Keywords
Anogenital mammary-like glands
Benign adnexal tumours
Hidradenoma papilliferum
Vulvar adnexal tumours
Vulvar hidradenomas
INTRODUCTION
The vulvar skin and modified mucosa are rich in pilosebaceous units, in addition to apocrine, eccrine and anogenital mammary-like glands. It is not surprising that both benign and malignant neoplasms originating from these adnexal structures are found in the vulva. Hidradenoma papilliferum (HP) is the most prevalent benign vulvar adnexal neoplasms, accounting for 60% of benign lesions and 42% of all vulvar adnexal neoplasms. It arises from anogenital mammary-like glands. Other benign lesions include cysts, tubular adenoma, poroma and spiradenoma.[1]
Here, we are describing the cases that emphasise the distinct clinical features and therapeutic approaches for two women, who were diagnosed with vulvar hidradenomas.
CASE REPORTS
Case 1
A 45-year-old woman presented with a painless vulval lesion of 7 years of duration. It was gradually increasing in size. There was no history of treatment taken for the same. She did not have any known comorbidities. Her sister had cervical cancer. Upon examination, a well-defined, flesh to redcoloured nodule, measuring 1 × 1 cm, was observed on the outer aspect of the right labia minora.
The nodule was firm and non-tender and had a slightly eroded surface, with no palpable regional lymph nodes [Figure 1].
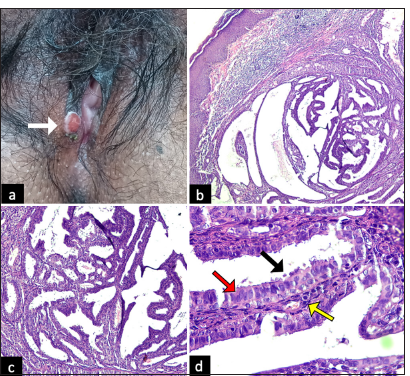
- (a) Gross appearance of the vulvar lesion (white arrow): Solitary, well-defined, flesh to red-coloured, firm nodule, measuring 1 × 1 cm, with slightly eroded surface on the right labia minora. (b) Scanner view (×4) (Haematoxylin and Eosin) showing a dermal cystic adnexal tumour with numerous papillary projections; (c) Low-power view (×10) (Haematoxylin and Eosin) showing papillary projections with cystic spaces. (d) High-power view (×40) (Haematoxylin and Eosin) showing numerous papillary projections lined by a peripheral layer of myoepithelial cells (yellow arrow) and a luminal layer of tall columnar cells (red arrow) showing decapitation of secretion (black arrow).
Pyogenic granuloma, vulvar adnexal tumour and donovanosis were considered as differential diagnoses.
The vulvar mass was completely excised by a simple elliptical excision with single layer closure using simple interrupted non-absorbable nylon monofilament (Ethilon) 5-0 sutures. Histopathological examination identified a dermal cystic adnexal tumour characterised by multiple papillary processes bordered by a luminal layer of tall columnar cells and a peripheral layer of myoepithelial cells displaying decapitation of secretion. This leads us to the diagnosis of HP. The patient required no further treatment and had an uneventful clinical course.
Case 2
A 38-year-old woman presented with an asymptomatic nodule on her vulva of 2-year duration. Her past history and family history were unremarkable.
Genital examination revealed a single, well-circumscribed, smooth-surfaced raised lesion measuring 4 × 4 mm, with focal ulceration. It was firm, nodular lesion, without regional lymphadenopathy. Excisional biopsy of the lesion was done, which showed comparable picture as in the first case [Figure 2].
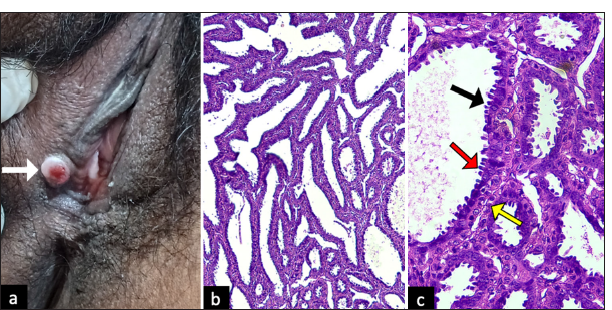
- (a) Gross appearance of the vulvar lesion (white arrow): a well-circumscribed, flesh to red-coloured, nodule, with eroded surface on the right labia minora. (b) Low-power view (×10) (Haematoxylin and Eosin) showing papillary projections with cystic spaces. (c) High-power view (×40) (Haematoxylin and Eosin) showing numerous papillary projections lined by a peripheral layer of myoepithelial cells (yellow arrow) and a luminal layer of tall columnar cells (red arrow) showing decapitation of secretions (black arrow).
DISCUSSION
In 1878, Worth published the initial report on HP. It is the most common benign neoplasm of vulvar adnexa. Initially classified as apocrine tumour, it is now considered as adenoma of mammary-like anogenital glands.
The exact cause of this condition remains unknown. Although few human papillomavirus (HPV) types have been detected in lesion tissues, HPV does not appear to be a causative factor.
It is most commonly reported in middle-aged women, with no cases documented in pre-pubertal individuals.[2] It typically presents as a slow-growing, well-defined, firm nodule in the anogenital region, ranging in colour from flesh to red. It is usually asymptomatic, solitary and <1 cm in diameter, although ulceration can occasionally occur, leading to itching and bleeding.
Baker et al.[1] noticed that the predilection sites were labia minora (50%), labia majora (40%), fourchette (7%) and clitoris (3%). Ectopic HP may infrequently manifest in areas of modified apocrine gland, including the breast, external auditory canal and eyelid.
Due to its rarity, HP in the vulvar region presents a diagnostic challenge, often leaving physicians with limited experience in recognising it. There are several differential diagnoses to consider, including squamous cell carcinoma, basal cell carcinoma and Paget’s disease[3] [Table 1].
| Differentials | Clinical features | Dermoscopic findings | Histopathological findings |
|---|---|---|---|
| Hidradenoma papilliferum | Asymptomatic nodules on vulva in middle-aged women | Central brown to greyish-blue non-pigmented regions encircled by speckled and irregular serpiginous telangiectasias or glossy white areas | Dermal cystic adnexal tumour with numerous papillary projections lined by a peripheral layer of myoepithelial cells and a luminal layer of tall columnar cells displaying decapitation of secretion |
| Squamous cell carcinoma | In sixth decade, solitary nodule with pruritus, ulceration, pain, bleeding. Associated with HPV infection | Compact irregular white areas without any vascular pattern | Downwards proliferation and invasion by dysplastic keratinocytes, horns and keratin pearls |
| Basal cell carcinoma | Rare, Seventh- eighth decade, aymptomatic pigmented nodule or erythematous plaque, pruritus and bleeding. Associated with chronic irritation, irradiation | Arborising vessels, blue ovoids, blue globules, white shiny structures | Aggregates of basaloid cells with peripheral palisading and clefts between the aggregates and the stroma |
| Melanoma | Whites, 5-7th decade. A pigmented macule and nodule which may ulcerate or bleed | Presence of varied colours, such as blue, grey, white, red and a whitish veil | Nests of atypical melanocytes along the dermo-epidermal junction, spindle-shaped atypical melanocytes in the dermis. IHC markers S100B, HMB45, Melan A |
| Papillary adeno-carcinoma | Rare, aggressive tumour with regional lymph node metastasis, presents with asymptomatic flesh coloured nodule on vulva | - | Irregular, invasive growth patterns with cellular atypia and lacks encapsulation, apocrine secretion and a double-layered structure |
| Syringocystadenoma papilliferum | Single or multiple erythematous papules with a cerebriform surface arranged linearly, may become warty, commonly associated with nevus sebaceous | A central yellowish depression, with polymorphous vessels and peripheral pinkish-white rim of hairpin vessels. | Cystic papillary invaginations of pseudo-stratified epithelium extending into lower dermis, enclosing stroma densely infiltrated with plasma cells |
| Syringoma | Typically multiple and bilaterally symmetrical, flesh coloured to yellow papules, common in young females | Shiny whitish-yellow oval to round structures on pink background | Sclerotic stroma containing epithelial cells arranged in nests, cords and tubules. (comma-shaped or tadpole appearance) |
| Extramammary paget disease | 6-8th decades of life, erythematous, well-demarcated plaques in anogenital region that may become erosive, scaly or eczematous | Milky-red/white structureless areas, polymorphous and glomerular vascular patterns, shiny white lines and pigmentary structures | Paget’s cells in stratum basale arranged singly or in clusters (expressing CK7 and CEA on special stains) |
HPV: Human papillomavirus, IHC: Immunohistochemical, HMB45: Human melanoma black, CEA: Carcinoembryonic antigen
Giorgi et al.[3] observed central greyish-blue non-pigmented regions on dermoscopy and encircled by speckled and irregular serpiginous telangiectasias or glossy white zones. In contrast, Tosti et al. noted that the dermoscopic findings of HP are polymorphic and not definitive for diagnosis. Although it is useful for differential diagnosis, histopathology remains the definitive diagnostic tool.[4] The absence of dermoscopy in both cases is a limitation of our case report.
The tumour generally has a favourable prognosis, with recurrences or malignant transformation being extremely rare. There are a few documented cases of ductal carcinoma in situ or squamous differentiation associated with HP. Vulvar adeno-squamous carcinomas, regardless of their origin, tend to have a poorer prognosis. The preferred treatment is local excision. Other treatment options include cryotherapy, radiofrequency or ablative laser.[5]
CONCLUSION
When assessing an adult female with a nodular lesion in the anogenital area, HP should be considered alongside other conditions such as sexually transmitted diseases and various benign and malignant tumours.
Although hidradenomas typically have a favourable prognosis and malignant transformation is uncommon, it is crucial to recognise that not all hidradenomas are benign. Therefore, even if vulvar nodules appear benign and have been present for a long time, prompt excisional biopsy is strongly advised.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship:
Nil.
References
- Vulvar Adnexal Lesions: A 32-year, Single-institution Review from Massachusetts General Hospital. Arch Pathol Lab Med. 2013;137:1237-46.
- [CrossRef] [PubMed] [Google Scholar]
- Hidradenoma Papilliferum of the Vulva: A Dermoscopic Challenging Diagnosis. An Bras Dermatol. 2023;98:546-8.
- [CrossRef] [PubMed] [Google Scholar]
- Vulval Hidradenoma Papilliferum: A Clinical and Dermoscopic Study. Clin Exp Dermatol. 2020;45:1035-9.
- [CrossRef] [PubMed] [Google Scholar]
- Vulvar Adenosquamous Carcinoma Arising in a Hidradenoma Papilliferum, with Rapidly Fatal Outcome: Case Report. Gynecol Oncol. 1989;35:395-8.
- [CrossRef] [PubMed] [Google Scholar]







