Translate this page into:
Painful Papules on the Pinna
*Corresponding author: Arun C. Inamadar, Department of Dermatology, Venereology and Leprosy, Shri B M Patil Medical College Hospital and Research Centre, BLDE (Deemed to be University), Vijayapur, Karnataka, India. aruninamadar@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Adya KA, Inamadar AC. Painful Papules on the Pinna. Indian J Postgrad Dermatol. 2024;2:60-2. doi: 10.25259/IJPGD_85_2023
Dear Editor,
An elderly male presented with moderately painful lesions on his right ear from the past 8–10 months. Examination revealed a whitish discrete dome-shaped papule with central haemorrhagic crust and skin-coloured papules coalescing into linear plaque involving the helix of the right ear [Figure 1]. Polarised dermoscopy (DermLite™ DL3, 3Gen Inc., San Juan Capistrano, CA, USA) of the discrete whitish papule revealed thick white radial lines and structureless areas on a pinkish-white background with central thick white scales and red structureless area. The adjoining coalesced skin-coloured papules revealed yellow-orange and yellow-white structureless areas over a pink background [Figure 2]. Histopathology of the whitish dome-shaped papule revealed hyperkeratosis with red blood cell aggregates in the centre, along with acanthosis and hypergranulosis with irregularly elongated and fused rete ridges. The dermis overlying the cartilage showed dense inflammatory infiltrate and few capillary proliferations [Figure 3]. The clinical, dermoscopic and histopathological features established the diagnosis of chondrodermatitis nodularis chronica helicis.

- Discrete whitish papule and coalesced skin-coloured papules on the right helix.

- Dermoscopy of the whitish papules showing thick white radial lines and structureless areas (black arrow) along with central white scales and red structureless area (blue arrow). The adjoining coalesced papules show yellow-orange (red arrow) and yellow-white (green arrow) structureless area over a pinkish background (Polarised, ×10).
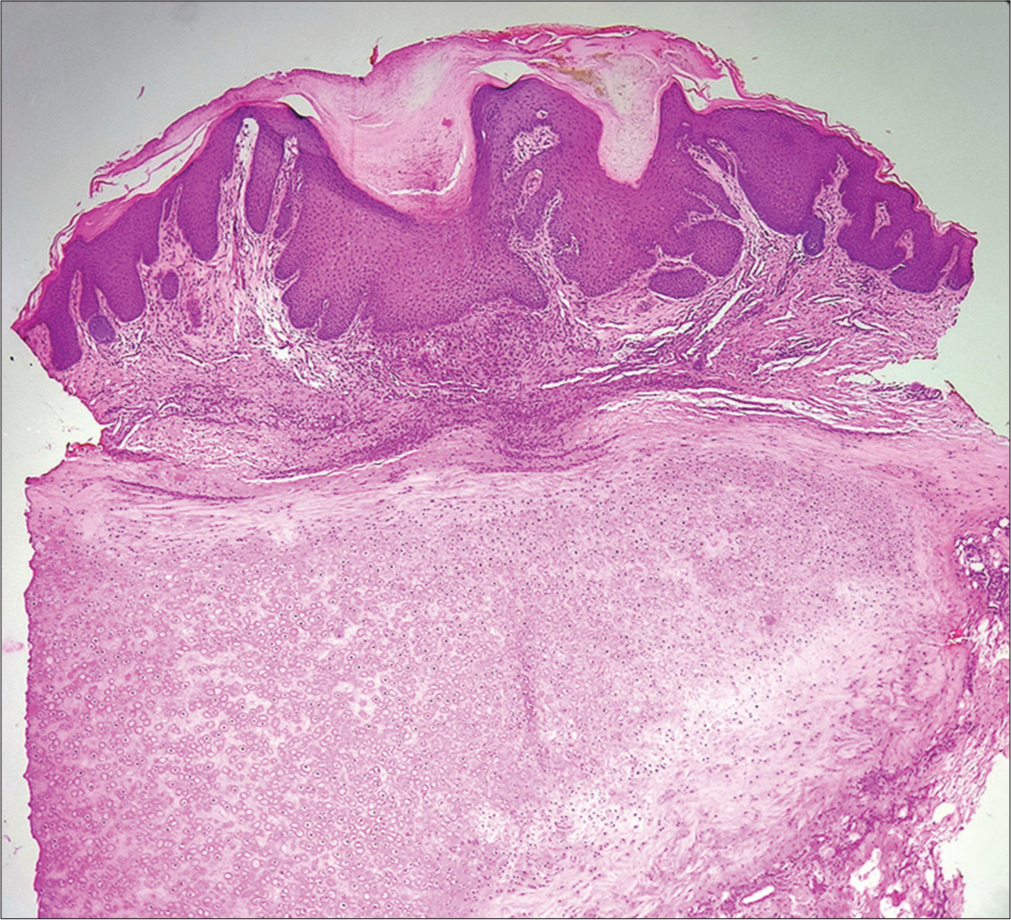
- Photomicrograph showing central hyperkeratosis with haemorrhage along with acanthosis and irregularly elongated and fused rete ridges. The dermis shows dense inflammatory infiltrate with capillary proliferation (H and E, ×10).
Chondrodermatitis nodularis chronica helicis or chondrodermatitis nodularis helicis (CNH, Winkler disease) is a benign inflammatory disorder affecting middle aged to elderly men. The classical site of occurrence is the highest point of the helix, frequently unilateral. Clinically, CNH presents with single or multiple erythematous to skin-coloured papules or nodules, often with central crusted umbilication. It is often associated with tenderness and nocturnal pain. Chronic recurrent pressure due to various causes, such as sleeping on one side and use of headgears or headphones is commonly attributed in CNH. Aberrations such as protruding pinna pre-dispose and inherent factors such as thinner skin overlying the ear cartilage with less subcutaneous fat and blood supply potentiate the development of CNH following trauma. Apart from pressure, chronic photodamage or chronic cold exposure leads to vasculopathy and chronic ischaemic damage to the skin and cartilage that incites granulomatous inflammation. Treatment of CNH is primarily aimed at removal of the inciting factor(s) responsible for chronic pressure. Pharmacological treatment options include topical/intralesional steroids, topical calcium channel blockers and nitroglycerine. Cases refractory to these modalities can be managed surgically or with electrocautery and lasers.[1,2]
As to the dermoscopy of CNH, observed features resemble those of squamous cell carcinoma (SCC) – white structures and structureless areas, keratin, haemorrhage and atypical vessels.[3,4] García-García et al. described a unique pattern of thick white radial lines converging onto the centre of the lesion formed by a yellow-brown clod representing crusted erosion. This pattern was found to be statistically specific for CNH compared to SCC and basal cell carcinoma (BCC).[3] An almost identical pattern was noted in the index case. Features noted by Morgado-Carrasco et al. were indistinguishable from SCC.[4]
Histopathologically, CNH is characterised by central ulceration with scaling and haemorrhagic crust with adjoining acanthosis, hypergranulosis and irregularly elongated rete ridges. The dermis beneath the ulceration shows fibroplasia, granulomatous infiltrate and vascular proliferation.[2] As to the dermoscopic-histopathologic correlation, the white lines and structureless areas correspond to acanthosis and the thick scales with red structureless area to the hyperkeratosis with haemorrhage. In addition to the pattern described by García-García et al.,[3] we also noted yellow-orange structureless areas in the skin-coloured papules of our case. This feature possibly corresponds to the granulomatous inflammation associated with CHN.[5] This feature, when present, may additionally help in distinguishing CNH from SCC or nodular BCC.
To conclude, CNH is a benign inflammatory dermatosis of the middle-aged and elderly individuals bearing quite a resemblance with SCC and hence needs to be differentiated from the same. Before histopathological confirmation, dermoscopy (along with the clinical context) may aid in its diagnosis as well as in differentiating CNH from SCC.
Ethical approval
The research/study complied with the Helsinki Declaration of 1964.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Chondrodermatitis Nodularis Helicis In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482507 [Last accessed on 2023 Mar 01]
- [Google Scholar]
- Alterations of Collagen and Elastin In: Barnhill RL, Crowson AN, Magro CM, Pipekorn MW, eds. Dermatopathology (3rd ed). New York: McGraw Hill Companies, Inc.; 2010. p. :387-407.
- [Google Scholar]
- Dermoscopy of Chondrodermatitis Nodularis Helicis. Arch Dermatol Res. 2018;310:551-60.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic Features of Chondrodermatitis Nodularis Chronica Helicis: A Case Series. Dermatol Pract Concept. 2019;9:52-3.
- [CrossRef] [PubMed] [Google Scholar]
- Dermatoscopy of Cutaneous Granulomatous Disorders. Indian Dermatol Online J. 2021;12:34-44.
- [CrossRef] [PubMed] [Google Scholar]






