Translate this page into:
Syndromic and Aetiological Profile of Patients Attending STD Clinic during COVID-19
*Corresponding author: Geeti Khullar, Department of Dermatology and STD, Vardhman Mahavir Medical College and Safdarjung Hospital, Delhi, India. geetikhullar@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Dhattarwal N, Khullar G, Monga A, Bhargava A, Khunger N, Muralidhar S. Syndromic and Aetiological Profile of Patients Attending STD Clinic during COVID-19. Indian J Postgrad Dermatol. doi: 10.25259/IJPGD_198_2024
Abstract
Coronavirus disease 2019 (COVID-19) affected epidemiology of sexually transmitted diseases (STDs) across the world due to decreased clinic attendance and hampered delivery of services. This retrospective study was undertaken from January 2020 to December 2021 to assess epidemiological trends of patients attending STD clinic of Apex Regional STD centre in North India. Correlation between COVID-19 and STD cases was assessed and numbers of various STD cases during pandemic were compared to pre-pandemic numbers. 1653 patients were included in the study. The most common presentation was vaginal discharge, followed by genital warts and genital ulcer. Correlation between STD and COVID-19 cases was not statistically significant. Statistically significant decrease in cases of non-gonococcal urethritis and syphilis was noted. This decrease could be either due to reduced disease transmission during COVID-19 or reduced clinic attendance which needs further evaluation.
Keywords
Coronavirus disease 2019
Epidemiology
Sexually transmitted diseases
INTRODUCTION
Coronavirus disease 2019 (COVID-19) affected close to 640 million worldwide.[1] Before COVID-19, the number of new cases of sexually transmitted diseases (STDs) was increasing across the world. According to the Centers for Disease Control and Prevention (CDC), 30% increase in reported cases of chlamydia, gonorrhoea and syphilis in the United States of America (USA) was seen between 2015 and 2019.[2] A rising trend of viral STDs and syphilis was also observed during 2014–2018 in India.[3] A 20% annual increase in all mandatory notifiable STDs was seen in Spain for the past 5 years before the pandemic.[4] Fear of contracting COVID-19 and lockdown restrictions affected sexual behaviour of patients as well as their hospital visits. In a study from the USA, 54% and 84% reduction in the number of STD clinic visits was seen in the COVID-19 evolving and plateau phase, respectively.[5] 40% reduction in the total number of consultations was seen during lockdown in a study from Australia.[6] Utilisation of STD resources for COVID-19 testing, vaccination and treatment presented additional barriers for patients needing STD care and services. 45% STD health department respondents reported disruptions in laboratory testing.[7] The impact of pandemic was different on different STDs. While some researchers found a sharp decrease in all STDs after the implementation of lockdown, others found no significant decrease in syphilis and gonorrhoea reporting from pre-lockdown to lockdown phase.[8] Hence, we undertook this study to examine the effect of COVID-19 on the epidemiology of various STDs.
MATERIALS AND METHODS
This hospital-based, retrospective study was conducted from January 2020 to December 2021. Clinical and demographic details were recorded from pre-designed datasheets of the STD clinic during pandemic (2020–2021). Unpaired t-test and P-value were calculated to compare diseases during 2 years of COVID-19 and pre-COVID-19. STD cases were also correlated with COVID-19 cases and peaks using the Spearman correlation coefficient.
RESULTS
The most common age group was 21–40 years and females outnumbered males [Supplementary Table 1]. Presenting complaints and final diagnoses are in Table 1.
| Diagnosis | 2020 | 2021 | ||||
|---|---|---|---|---|---|---|
| Male | Female | Total | Male | Female | Total | |
| Vaginal discharge | - | 174 | 174 | - | 340 | 340 |
| Candida | - | 88 | 88 | - | 195 | 195 |
| Trichomonas | - | 5 | 5 | - | 7 | 7 |
| Bacterial vaginosis | - | 22 | 22 | - | 55 | 55 |
| Others (Escherichia coli, Staphylococcus aureus, Proteus) | - | 5 | 5 | - | 5 | 5 |
| Gonococcal cervicitis | - | 1 | 1 | - | 0 | 0 |
| Non-gonococcal cervicitis | - | 1 | 1 | - | 1 | 1 |
| No organism isolated | - | 52 | 52 | - | 77 | 77 |
| Genital warts | 58 | 44 | 102 | 99 | 66 | 165 |
| Genital ulcer | 66 | 25 | 91 | 122 | 45 | 167 |
| Herpes | 65 | 24 | 89 | 120 | 43 | 163 |
| Chancroid | 0 | 1 | 1 | 2 | 2 | 4 |
| Primary syphilis | 1 | 0 | 1 | 0 | 0 | 0 |
| Syphilis | 65 | 29 | 94 | 97 | 40 | 137 |
| Primary syphilis | 1 | 0 | 1 | 0 | 0 | 0 |
| Secondary syphilis | 8 | 4 | 12 | 26 | 10 | 36 |
| Latent syphilis | 56 | 25 | 81 | 71 | 30 | 101 |
| Molluscum contagiosum | 26 | 35 | 61 | 39 | 53 | 92 |
| Balanoposthitis | 68 | - | 68 | 84 | - | 84 |
| Infectious (Candida) | 18 | - | 18 | 24 | - | 24 |
| Non-infectious | 50 | - | 50 | 60 | - | 60 |
| Urethral discharge | 19 | - | 19 | 60 | - | 60 |
| Gonococcal | 14 | - | 14 | 52 | - | 52 |
| Non-gonococcal | 5 | - | 5 | 8 | - | 8 |
| Total | 257 | 351 | 608 | 416 | 629 | 1045 |
STD: Sexually transmitted disease
Overall, the most common presenting complaint was vaginal discharge accounting for 49.6% and 54% cases among females in 2020 and 2021, respectively. In males, the most common presenting complaint was redness or itching, burning sensation over the penis (balanoposthitis) in 2020 (26.5%) and genital ulcer in 2021 (29.3%). Candidiasis was the most frequently implicated aetiology of vaginal discharge (55.3%).
There was a decline in STD cases in months with very high COVID-19 cases, but the correlation was not statistically significant (Spearman’s correlation coefficient - 0.2, P = 0.327) [Figure 1].
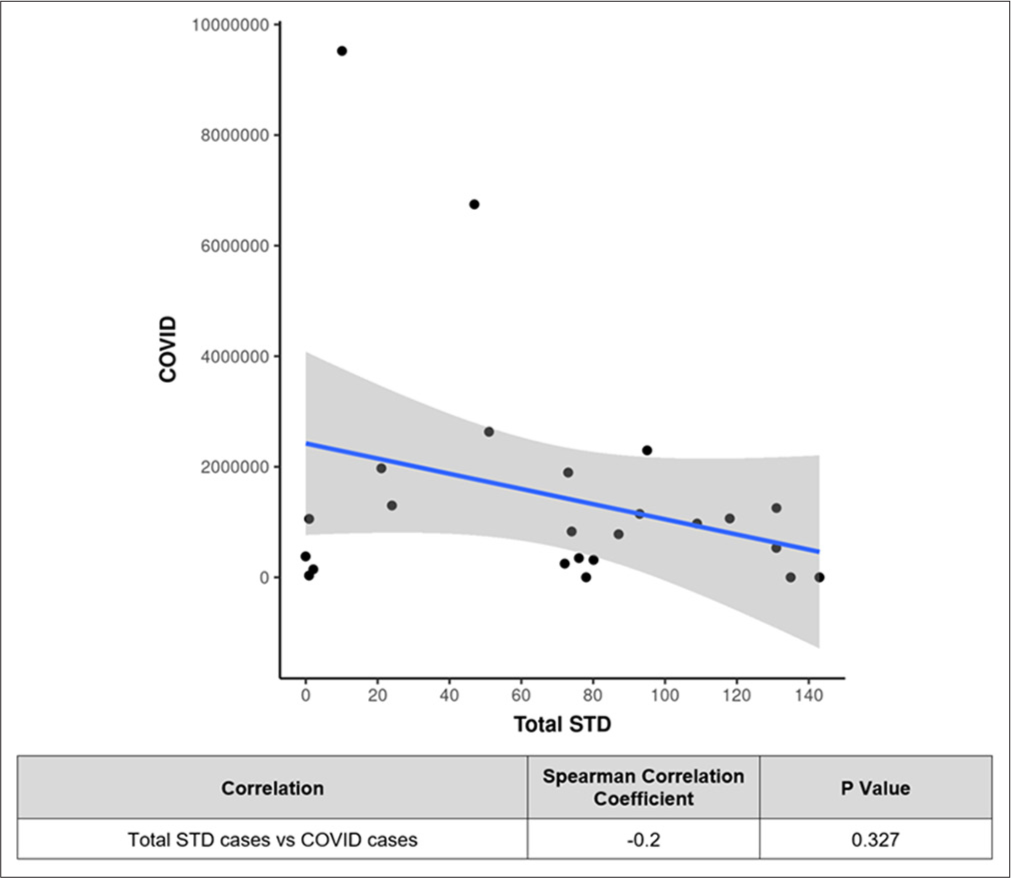
- Statistical correlation between coronavirus disease 2019 cases and sexually transmitted diseases (STD) cases using Spearman’s coefficient formula. Black dots represent total COVID cases and STD cases and blue line indicates the corelation between these numbers.
On comparing the various diseases pre-pandemic and during COVID-19 pandemic, there was a statistically significant decrease in the cases of non-gonococcal urethritis and syphilis [Table 2].
| Mean pre-COVID-19 | Mean during COVID-19 | % decrease/increase | P-value | |
|---|---|---|---|---|
| Vaginal discharge | 391 | 257 | −34.3 | 0.297 |
| Candida | 148 | 142 | −4 | 0.925 |
| Trichomonas | 12 | 6 | −50 | 0.115 |
| Bacterial vaginosis | 66 | 39 | −40.9 | 0.243 |
| Others/No organism | 165 | 66 | −60 | 0.036* |
| Urethral discharge | 65 | 40 | −38.5 | 0.355 |
| Gonococcal | 38.5 | 33 | −14.3 | 0.801 |
| Non-gonococcal | 26.5 | 7 | −73.6 | 0.034* |
| Herpes | 229.5 | 76 | −66.9 | 0.108 |
| Chancroid | 4.5 | 3 | −33.3 | 0.564 |
| Syphilis | 203 | 116 | −42.9 | 0.032* |
| Warts | 261 | 134 | −48.7 | 0.065 |
DISCUSSION
The COVID-19 pandemic brought great challenges to the world and the measures taken in response to the situation had consequences on the epidemiology of STDs. The fear of contracting the virus coupled with social confinement measures led to less people attending STD clinics. Berzkalns et al. noted that the sexual health clinic visits during lockdown in 2020 were 55% lower than in 2019.[9] In addition, some studies also found that the more stringent the control measures, the more the decline in reported STD cases.[10] Consequently, there was a sharp decline in gonorrhoea cases in the United Kingdom,[11] syphilis cases in Italy and USA,[12,13] gonorrhoea and syphilis cases in Greece and Spain[14,15] and HIV, hepatitis B and C, gonorrhoea and syphilis cases in China.[10] A sharp decline in STD clinic attendance and numbers of all STDs was noted in our study as well.
Diversion and reassignment of resources led to reduced hours of operation and disruptions in testing in STD clinics which hampered preventive counselling, early diagnosis and treatment. However, there was no disruption in the services of our STD clinic during the pandemic.
Lockdown restrictions on social gatherings reduced seeking of casual sexual partners and high risk sexual behaviour. Moreover, there were concerns about contracting COVID-19 infection from the partner. We did not assess the sexual behaviour and frequency in our patients but a study from Amsterdam showed a 73% reduction in the number of casual sex partners of men who have sex with men.[16] Li et al. observed a decrease in the number of sexual partners and sexual frequency during the lockdown period in China, especially among people with high-risk sexual behaviours.[17]
Some of the clients sought syndromic management through telemedicine consultations during this period, a practice supported by CDC recommendations.[18]
The present study was carried out to examine the epidemiological trends of patients attending STD clinic during COVID-19 pandemic and compare it with pre-pandemic period. Decline in STD clinic attendance and numbers of all STDs was noted during COVID-19 pandemic in contrast to the previous increasing trend every year. On correlating monthly STD cases with COVID-19 cases, no statistically significant trend was noted. Nationwide lockdown was announced on 24th March 2020 followed by gradual lifting of lockdown from June 1, 2020, to July 31, 2020.[19] Daily life and other services slowly became normal and the number of STD cases increased in the year 2021; however remained lower than in previous years. This is in contrast to findings from China, where after sharp decline of STD reported cases, the case numbers recovered quickly and then returned to normal.[11] A similar trend was also reported in the USA.[20]
In the study from China, after a rapid decline syphilis had rapid rebound but the recovery of gonorrhoea’s case number was relatively slow.[10] In another study, there was no significant difference in cases of syphilis reporting during lockdown or post-lockdown but rebound increase in daily median chlamydia and gonorrhoea case reporting post-lockdown.[8] In our study, statistically significant reduction in the cases of non-gonococcal urethritis and syphilis compared to pre-pandemic numbers was noted. The exact mechanism leading to statistically significant decline in only few STDs still remains unanswered as contrasting findings were observed in different studies and need further evaluation.
We found only one other study from North-east India on epidemiology of STDs during COVID-19 pandemic. A decline in overall number of patients was seen but in contrast to our findings, herpetic genital ulcer was the most common STD, followed by syphilis and urethral discharge.[21]
Limitations of our study include retrospective study design and lack of polymerase chain reaction to identify causative organisms.
CONCLUSION
Decreased STD clinic attendance was noted during COVID-19. However, correlation between STD cases and COVID-19 cases was not significant. Statistically significant decline was noted in non-gonococcal urethritis and syphilis compared to pre COVID-19 numbers.
Ethical approval:
Since it was retrospective observational study, institutional ethics approval was not taken.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest:
Dr. Geeti Khullar, Dr. Niti Khunger are on the Editorial Board of the Journal.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Our World in Data. 2022. Available from: https://ourworldindata.org/explorers/coronavirus-data-explorer [Last accessed on 2022 Dec 18]
- [Google Scholar]
- Centers for Disease Control and Prevention. 2021. Available from: https://www.cdc.gov/nchhstp/newsroom/2021/2019-std-surveillance-report-press-release.html#:~:text=the%20newly%20released%202019%20std,stds%20between%202015%20and%202019 [Last accessed on 2022 Dec 18]
- [Google Scholar]
- Trends of Sexually Transmitted Infections in A Tertiary Care Center: A 5 Year's Analysis. Int J Dermatol Venereol Lepr Sci. 2021;4:13-7.
- [CrossRef] [Google Scholar]
- The Impact of the COVID-19 Pandemic on Sexually Transmitted Infections Surveillance Data: Incidence Drop or Artefact? BMC Public Health. 2021;21:1637.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of the COVID-19 Pandemic on Sexually Transmitted Infection Clinic Visits. Sex Transm Dis. 2021;48:e5-7.
- [CrossRef] [PubMed] [Google Scholar]
- Sexually Transmitted Infection Diagnoses and Access To A Sexual Health Service before and after the National Lockdown for COVID-19 in Melbourne, Australia. Open Forum Infect Dis. 2020;8:ofaa536.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of the COVID-19 Pandemic on Centers for Disease Control and Prevention-Funded Sexually Transmitted Disease Programs. Sex Transm Dis. 2022;49:e61-3.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of COVID-19 Lockdowns on Sexual Health Care Utilization and STD Reporting, Maricopa County. Inquiry. 2021;58:469580211055583.
- [CrossRef] [PubMed] [Google Scholar]
- Decreases in Reported Sexually Transmitted Infections During the Time of COVID-19 in King County, WA: Decreased Transmission or Screening? Sex Transm Dis. 2021;48:S44-9.
- [CrossRef] [PubMed] [Google Scholar]
- The Epidemic of Sexually Transmitted Diseases Under the Influence of COVID-19 in China. Front Public Health. 2021;9:737817.
- [CrossRef] [PubMed] [Google Scholar]
- Gonorrhoea During COVID-19 in London, UK. Sex Transm Infect. 2021;97:622-3.
- [CrossRef] [PubMed] [Google Scholar]
- Is COVID-19 Affecting the Epidemiology of STIs? The Experience of Syphilis in Rome. Sex Transm Infect. 2021;97:78.
- [CrossRef] [PubMed] [Google Scholar]
- Reporting of Sexually Transmitted Infections During the COVID-19 Pandemic. Sex Transm Infect. 2021;97:101-2.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of COVID-19 Pandemic On STIs in Greece. Sex Transm Infect. 2022;98:70.
- [CrossRef] [PubMed] [Google Scholar]
- Social Distancing to Combat COVID-19 Led to a Marked Decrease in Food-borne Infections and Sexually Transmitted Diseases in Spain. J Travel Med. 2020;27:taaa134.
- [CrossRef] [PubMed] [Google Scholar]
- Sexual Behavior and its Determinants During COVID-19 Restrictions among Men Who Have Sex With Men in Amsterdam. J Acquir Immune Defic Syndr. 2021;86:288-96.
- [CrossRef] [PubMed] [Google Scholar]
- Challenges in the Practice of Sexual Medicine in the Time of COVID-19 in China. J Sex Med. 2020;17:1225-8.
- [CrossRef] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. 2020. Available from: https://public4.pagefreezer.com/browse/cdc%20covid%20pages/11-05-2022t12:30/https://www.cdc.gov/coronavirus/2019-ncov/hcp/telehealth.html [Last accessed on 2022 Dec 18]
- [Google Scholar]
- Wikipedia. 2022. Available from: https://en.wikipedia.org/wiki/COVID-19_lockdown_in_India [Last accessed on 2022 Dec 18]
- [Google Scholar]
- Impact of the COVID-19 Pandemic on Chlamydia and Gonorrhea Screening in the U.S. Am J Prev Med. 2021;61:386-93.
- [CrossRef] [PubMed] [Google Scholar]
- The Trend of STD in COVID Times-A Retrospective Hospital-based Study from Northeast India. IP Indian J Clin Exp Dermatol. 2022;8:43-6.
- [CrossRef] [Google Scholar]








