Translate this page into:
Quality of Life and Sexual Function in Women with Sexually Transmitted Infections/Reproductive Tract Infections: A Hospital-Based Study
*Corresponding author: Damini Verma, Department of Dermatology, Lady Hardinge Medical College and Hospitals, New Delhi, India. vdamini89@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Agrawal M, Garg T, Chander R, Verma D. Quality of Life and Sexual Function in Women with Sexually Transmitted Infections/Reproductive Tract Infections: A Hospital-Based Study. Indian J Postgrad Dermatol. doi: 10.25259/IJPGD_37_2024
Abstract
Objectives:
The study was conducted to assess the quality of life (QOL) and the sexual function in women with sexually transmitted infections (STIs)/reproductive tract infections (RTIs).
Materials and Methods:
A total of 60, females aged 18-45 years with symptoms of STIs/RTIs of more than 1-month duration were enrolled over a period of 1 year along with 60 healthy controls. The world health organization quality of life brief version (WHO)-QOL-BREF questionnaire and female sexual function index (FSFI) questionnaire were used to assess the QOL and sexual function in all the subjects.
Results:
Majority of the patients were diagnosed as candidal vulvovaginitis (n = 20, 33.33%), followed by bacterial vaginosis (16.67%). The mean scores (both WHO-QOL-BREF and FSFI scores) for all the domains as well as overall scores were higher in the control group as compared to the cases (P = 0.001). Both WHO-QOL-BREF scores and FSFI scores were lowest in mixed infection group (genital molluscum contagiosum and herpes genitalis).
Conclusion:
As both QOL and sexual function are adversely affected in women having STIs/RTIs, it should be an important part of patient management. A larger community-based study is required to confirm our findings so as to use QOL and female sexual function measures, in addition to other measures, in studies conducted to evaluate various treatment modalities in chronic and recurrent STIs/RTIs.
Keywords
Female sexual function index
Quality of life
Sexual function
Sexually transmitted infections
World Health Organization quality of life BREF score
INTRODUCTION
Sexually transmitted infections (STIs) are infections that spread primarily through sexual contact. Reproductive tract infections (RTIs) are a broad term that includes not only STIs but also other infections of the reproductive tract that are not transmitted through sexual contact. STIs/RTIs constitute a major public health problem for both developing and developed countries.[1] These are known to have a significant impact on physical, psychological and sexual health, adversely affecting quality of life (QOL). There has been a decline in bacterial STIs and a rise in viral STIs over the past few decades. This could be due to the widespread use of antibiotics, use of barrier methods of contraception and adoption of safer sexual behaviour due to the risk perception of human immunodeficiency virus (HIV).[2] There has been a greater impact of viral STIs on the QOL of patients due to their chronicity.[3] However, data are scarce, especially in the Indian setting, regarding QOL in other STIs/RTIs.[2] The World Health Organization (WHO)-QOL-BREF Questionnaire is an instrument developed by the WHO to analyse the QOL across patient groups in different countries and cultures.[4]
Female sexual function index (FSFI) questionnaire is a brief questionnaire used to measure the sexual functioning in women in which various domains of sexual functioning (desire, arousal, lubrication, orgasm, satisfaction and pain) are studied.[5]
Very few studies have been done on this topic and these have focused mainly on selected infections.
MATERIALS AND METHODS
This was a hospital-based observational study in which a total of 60, married consenting females aged 18-45 years attending the Suraksha clinic in the department of Dermatology at a tertiary care centre, with symptoms of STIs/RTIs of more than 1-month duration or those with chronic/recurrent infections with history of symptom/clinical activity in the past 1 month were enrolled. An equal number of healthy married consenting women were taken as controls in the study. They were healthy attendants of patients or patients who sought treatment in dermatology outpatient department for other complaints, but did not give any history suggestive of STIs/RTIs. Permission from the institutional ethics committee was taken.
Clinical details including their demographic data, presenting complaint(s), history and a detailed examination were recorded. Relevant investigations were carried out in addition to HIV 1 and 2 testing (by enzyme-linked immunosorbent assay method) and venereal disease research laboratory testing.
WHO-QOL-BREF questionnaire was used to evaluate the QOL across four domains (physical, psychological, social and environment). It also includes two individually scored items about an individual’s overall perception of QOL and health. It consists of 26 items, each rated on a five-point Likert scale ranging from 1 to 5. Scores from all 4 domains were combined to produce a final score, which can range from 0 to 400, with higher scores indicating a better QOL. Sexual function was assessed for all participants using the FSFI questionnaire, which comprises 19 questions covering six domains: Desire, arousal, lubrication, orgasm, satisfaction and pain. These domains can be analysed both individually and as a whole, with the questions focusing on the participants’ sexual feelings and responses over the past 4 weeks. The total FSFI score is calculated by summing the scores from the six domains, with higher scores indicating better sexual function, ranging from 2 to 36.
Statistical analysis
The statistical analysis was conducted using the Statistical Package for the Social Sciences software version 17.0. Categorical variables were presented as frequencies and percentages and were analysed using the Chi-square test, with P < 0.05 considered statistically significant. Quantitative variables were expressed as mean ± standard deviation (SD) and assessed using the t-test, with significance set at P < 0.05. Differences amongst group means were evaluated using analysis of variance, with P < 0.05 considered statistically significant.
RESULTS
Mean age of cases was 30.53 ± 7.21 years and that of controls was 30.70 ± 5.82. Majority of the cases (n = 28, 46.67%) and controls (n = 37, 61.67%) were literate and had done schooling partially. Mean duration of the symptoms was 6.84 ± 10.32 months and majority of the patients had it for <6 months (n = 43, 71%).
Menstrual and reproductive history
Fifty-six cases gave a normal menstrual history and 4 cases complained of irregular menses. History of infertility was present in 7 (11.67%) cases and 1 (1.67%) control. Similarly history of use of contraceptives were found in greater number in cases (32 [53.3%]) than controls (29 [48.3%]). However, history of unplanned pregnancies was more in controls and no differences were observed between the cases and controls in terms of history of abortions. There were no statistically significant differences between the two groups in any of the parameters.
Past history
A detailed history elicited from the cases and controls revealed that a higher number of women with STIs/RTIs gave history of tattooing, multiple sexual partners, commercial sex work, orogenital/anogenital intercourse and drug addictions as compared to healthy controls [Table 1].
| History | Number of cases (n=60) Number/% | Number of controls (n=60) Number/% |
|---|---|---|
| Sociodemographic history | ||
| Age group (years) | ||
| 18–25 | 20 (33.33) | 9 (15) |
| 26–30 | 13 (21.67) | 25 (41.67) |
| 31–35 | 13 (21.67) | 16 (26.67) |
| 36–40 | 10 (16.67) | 5 (8.33) |
| 41–45 | 4 (6.67) | 5 (8.33) |
| Education level | ||
| Illiterate | 15 (25) | 10 (16.67) |
| Partial/incomplete schooling | 28 (46.67) | 37 (61.67) |
| Complete schooling | 9 (16) | 11 (18.33) |
| Educated beyond schooling | 8 (13.33) | 2 (3.33) |
| Menstrual and reproductive history of cases and controls | ||
| Abnormal menstrual history | 4 (6.67) | 2 (3.33) |
| History of infertility | 7 (11.67) | 1 (1.67) |
| History of abortions | 8 (13.33) | 8 (13.33) |
| Use of contraceptives | 32 (53.33) | 29 (48.33) |
| Condoms | 22 (36.67) | 28 (46.67) |
| Intrauterine devices | 4 (6.67) | 0 (0) |
| Tubal ligation | 5 (8.33) | 1 (1.67) |
| Oral contraceptive pills | 1 (1.67) | 0 (0) |
| History of unplanned pregnancies | 2 (3.33) | 5 (8.33) |
| Past history | ||
| History of tattooing | 11 (18.33) | 6 (10) |
| History of blood transfusion | 5 (8.33) | 5 (8.33) |
| >1 sexual partner | 6 (10) | 4 (6.67) |
| Correct and consistent method of barrier use | 20 (33.33) | 28 (46.67) |
| Commercial sex work | 1 (1.67) | 0 (0) |
| Anogenital/orogenital contact | 11 (18.33) | 9 (15) |
| Drug addictions (self/partner) | 1 (1.67) | 0 (0) |
| Age at the time of first sexual contact | ||
| <18 years | 20 (33.33) | 3 (5) |
| 18–25 years | 35 (58.33) | 54 (90) |
| 26–30 years | 5 (8.33) | 3 (5) |
| Frequency of sexual intercourse | ||
| 2–3 times/week | 13 (21.67) | 7 (11.67) |
| Once a week | 31 (51.67) | 44 (73.33) |
| Once in 2 weeks | 8 (13.33) | 7 (11.67) |
| Once a month | 7 (11.67) | 1 (1.67) |
| More than once a month | 1 (1.67) | 1 (1.67) |
Evaluation of quality of life by WHO-QOL-BREF score and sexual function by FSFI questionnaire
Majority of the patients were diagnosed as candidal vulvovaginitis (n = 20, 33.33%), followed by (16.67%) bacterial vaginosis. Genital warts, non-gonococcal cervicitis and herpes genitalis were detected in 8 (13.33%) patients each. Mixed infection (genital molluscum contagiosum and herpes genitalis) was seen in 1 (1.67 %) patient [Figure 1].
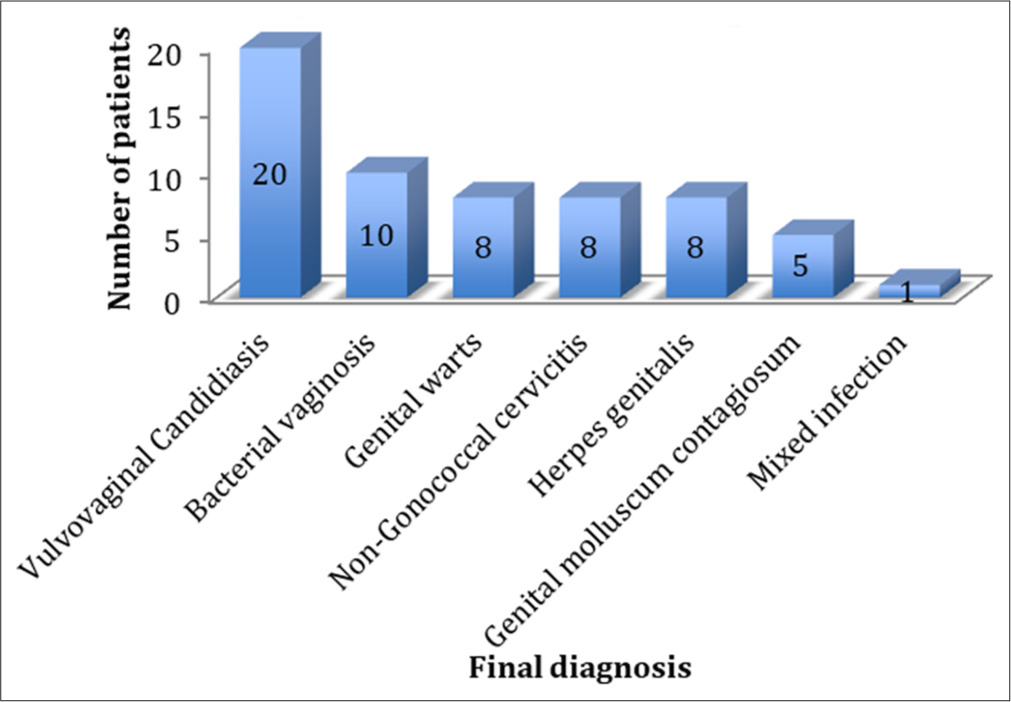
- Distribution of final diagnosis.
On evaluation of the WHO-QOL-BREF scores, it was found that the mean scores for all the domains as well as overall scores were lower in cases as compared to control group with a statistically significant difference (P = 0.001) [Table 2]. The mean scores for WHO-QOL-BREF were found to be the lowest in mixed infection group (144.00 ± 0), with second minimum in herpes genitalis group (160.38 ± 69.91) and maximum in genital molluscum contagiosum group (239.20 ± 77.25). However, statistically significant difference between mean scores of various STIs was seen only in the scores of physical domains (P = 0.038) [Table 3].
| Range of scores (cases) | Mean score of cases±SD | Range of scores (controls) | Mean score of controls±SD | P-value | |
|---|---|---|---|---|---|
| WHO-QOL-BREF scores of cases and controls | |||||
| Physical score | 19–88 | 57.43±18.94 | 31–94 | 78.33±15.17 | 0.001 |
| Psychological score | 19–100 | 52.50±20.04 | 38–100 | 80.35±14.95 | 0.001 |
| Social score | 6–100 | 50.53±22.50 | 44–100 | 78.95±10.69 | 0.001 |
| Environmental score | 13–88 | 48.98±17.72 | 44–100 | 78.00±13.34 | 0.001 |
| WHO-QOL-BREF | 57–369 | 209.33±67.29 | 176–394 | 315.63±48.41 | 0.001 |
| FSFI scores of cases and controls | |||||
| Desire | 1.2–6.0 | 2.817±1.46 | 1.2–6.0 | 4.190±1.42 | 0.001 |
| Arousal | 1.2–6.0 | 3.417±1.30 | 1.2–6.0 | 4.615±1.25 | 0.001 |
| Lubrication | 1.2–6.0 | 4.027±1.41 | 1.2–6.0 | 5.720±0.70 | 0.001 |
| Orgasm | 1.2–6.0 | 2.882±1.17 | 1.2–6.0 | 4.223±1.36 | 0.001 |
| Satisfaction | 1.2–6.0 | 3.438±1.34 | 1.2–6.0 | 4.552±1.48 | 0.001 |
| Pain | 1.2–6.0 | 3.258±1.61 | 3.6–6.0 | 5.767±0.61 | 0.001 |
| Total FSFI score | 7.2–36.6 | 19.838±6.55 | 12.0–36.0 | 29.067±5.17 | 0.001 |
WHO: World Health Organization, QOL: Quality of life, FSFI: Female sexual function index, SD: Standard deviation
| Disease | Mean physical domain scores±SD | Mean psychological domain scores±SD | Mean social domain scores±SD | Mean environmental domain scores±SD | Mean WHO-QOL-BREF scores±SD |
|---|---|---|---|---|---|
| Genital molluscum contagiosum n=5 | 65.00±14.95 | 48.80±26.19 | 65.00±21.47 | 60.40±22.27 | 239.20±77.25 |
| VVC n=20 | 58.25±19.77 | 57.30±21.63 | 46.90±26.06 | 47.95±17.53 | 208.50±70.29 |
| Genital warts n=8 | 60.00±13.55 | 57.78±15.09 | 57.00±16.68 | 51.44±15.76 | 229.67±50.37 |
| BV n=10 | 68.88±9.26 | 54.63±21.28 | 54.63±20.24 | 51.75±18.43 | 229.88±57.94 |
| Non gonococcal cervicitis n=8 | 57.22±20.21 | 52.22±17.85 | 50.11±21.68 | 47.22±16.36 | 206.78±67.34 |
| Herpes genitalis n=8 | 39.88±20.45 | 36.13±14.58 | 42.13±22.34 | 42.25±20.33 | 160.38±69.91 |
| Mixed (genital MC and herpes genitalis) n=1 | 31.00±0 | 44.00±0 | 31.00±0 | 38.00±0 | 144.00±0 |
| P-value | 0.038 | 0.275 | 0.500 | 0.677 | 0.258 |
WHO: World Health Organization, QOL: Quality of life, STI: Sexually transmitted infection, RTI: Reproductive tract infection, SD: Standard deviation, BV: Bacterial vaginosis, WHOQOL-BREF: World health organization quality of life brief version,VVC: Vulvovaginal candidiasis,
MC: Molluscum contagiosum
On analysis of FSFI scores, mean scores were higher in the control group as compared to cases, with a statistically significant difference [Table 2]. On comparison between the sexual function between various STIs/RTIs, lowest FSFI mean score was observed in the mixed infection group, 13.600 ± 0, with the second lowest in herpes genitalis group (15.975 ± 8.37), whereas the highest score was seen in genital warts with a mean score of 24.767 ± 6.81 [Table 4]. On analysing, the scores in individual sexual function domains between various STIs/RTIs, statistically significant difference was observed only in the scores of satisfaction (P = 0.026) and pain (P = 0.023) domains [Table 4]. Outcomes of FSFI and WHO-QOL-BREF scores were evaluated according to demographic characteristics in Table 5.
| Disease | Mean Desire scores±SD | Mean arousal scores±SD | Mean Lubrication scores±SD | Mean orgasm scores±SD | Mean satistfaction scores±SD | Mean pain scores±SD | Mean FSFI scores±SD |
|---|---|---|---|---|---|---|---|
| Genital molluscum contagiosum n=5 | 3.920±1.85 | 4.400±1.11 | 4.380±1.58 | 3.120±1.30 | 3.520±1.21 | 3.360±0.92 | 22.700±5.12 |
| Vulvovaginal candidiasis n=20 | 2.490±1.26 | 3.255±1.19 | 3.870±1.43 | 2.585±0.99 | 3.215±1.17 | 2.655±1.49 | 18.070±5.39 |
| Genital warts n=8 | 3.333±1.56 | 3.833±1.28 | 4.533±1.41 | 3.822±1.49 | 4.578±1.25 | 4.667±1.45 | 24.767±6.81 |
| Bacterial vaginosis n=10 | 2.775±1.35 | 3.300±1.54 | 4.087±1.56 | 3.000±1.28 | 3.950±1.59 | 3.600±1.28 | 20.713±6.58 |
| Non-gonococcal cervicitis n=8 | 2.867±1.63 | 3.600±1.00 | 4.311±0.72 | 2.800±0.77 | 3.333±1.14 | 3.689±1.59 | 20.600±5.18 |
| Herpes genitalis n=8 | 2.400±1.53 | 2.775±1.64 | 3.450±1.74 | 2.400±1.19 | 2.400±1.19 | 2.550±1.80 | 15.975±8.37 |
| Mixed (genital molluscum contagiosum and herpes genitalis) n=1 | 2.400 | 2.400 | 2.400 | 2.800 | 2.400 | 1.200 | 13.600 |
| P-value | 0.474 | 0.373 | 0.591 | 0.190 | 0.026 | 0.023 | 0.065 |
STI: Sexually transmitted infection, RTI: Reproductive tract infection, SD: Standard deviation, FSFI: Female sexual function index
| Parameter | n (%) | FSFI (mean scores±SD) | ||||||
| Desire | Arousal | Lubrication | Orgasm | Satisfaction | Pain | FSFI overall | ||
| Age of the cases (years) | ||||||||
| <30 years | 30 (50) | 3.01±2.83 | 3.53±1.43 | 4.14±1.47 | 3.01±1.29 | 3.46±1.38 | 3.21±1.72 | 20.38±7.52 |
| >30 years | 30 (50) | 2.62±1.27 | 3.33±1.71 | 3.91±1.35 | 2.75±1.05 | 3.41±1.33 | 3.30±1.50 | 19.29±5.48 |
| P-value | 0.49 | 0.62 | 0.53 | 0.39 | 0.88 | 0.82 | 0.52 | |
| Duration of presenting complaints (months) | ||||||||
| <6 months | 38 (63.33) | 2.64±1.53 | 3.25±1.53 | 3.90±1.59 | 2.86±1.28 | 3.36±1.47 | 3.33±1.78 | 19.36±7.37 |
| >6 months | 22 (36.67) | 3.10±1.33 | 3.69±1.07 | 4.24±1.01 | 2.90±0.98 | 3.56±1.13 | 3.12±1.29 | 20.65±4.86 |
| P-value | 0.24 | 0.23 | 0.37 | 0.89 | 0.58 | 0.63 | 0.46 | |
| Contraception | ||||||||
| None used | 28 (46.67) | 2.69±1.23 | 3.19±1.24 | 4.06±1.40 | 2.66±1.11 | 3.22±1.38 | 3.13±1.62 | 18.97±6.09 |
| Used | 32 (53.33) | 2.92±1.65 | 3.21±1.40 | 3.99±1.43 | 3.07±1.21 | 3.62±1.31 | 3.36±1.62 | 20.59±6.93 |
| P-value | 0.54 | 0.95 | 0.84 | 0.17 | 0.25 | 0.58 | 0.34 | |
| Condom usage | ||||||||
| Absent | 40 (66.67) | 2.68±1.35 | 3.27±1.28 | 3.97±1.37 | 2.67±1.11 | 3.26±1.43 | 3.07±1.62 | 18.95±6.37 |
| Present | 20 (33.33) | 3.09±1.66 | 3.69±1.33 | 4.12±1.50 | 3.3±1.22 | 3.78±1.10 | 3.62±1.57 | 21.61±6.70 |
| P-value | 0.30 | 0.24 | 0.69 | 0.04 | 0.15 | 0.21 | 0.13 | |
| Parameter | WHO-QOL-BREF (mean scores±SD) | Knowledge and awareness n (%) | ||||||
| Physical | Psychological | Social | Environmental | WHO-QOL- BREF overall | Heard of STI/RTI? | Aware of curability of STI/RTI? | ||
| Age of the cases (years) | ||||||||
| <30 years | 56.93±21.54 | 50.30±21.25 | 50.2±26.19 | 47.86±19.12 | 206.33±77.22 | 25 (41.67) | 13 (21.67) | |
| >30 years | 57.93±16.27 | 54.7±18.85 | 50.86±18.54 | 50.1±16.45 | 212.33±56.82 | 26 (41.33) | 9 (15) | |
| P-value | 0.83 | 0.39 | 0.91 | 0.62 | 0.773 | 1.000 | 0.42 | |
| Duration of presenting complaints (months) | ||||||||
| <6 months | 55.23±18.38 | 50.13±21.51 | 53±22.43 | 49±17.87 | 208.18±68.76 | 34 (56.67) | 14 (23.33) | |
| >6 months | 61.22±19.70 | 56.59±19.31 | 46.27±22.50 | 48.95±17.88 | 211±66.19 | 17 (28.33) | 8 (13.33) | |
| P-value | 0.24 | 0.24 | 0.26 | 0.99 | 0.87 | 0.71 | 0.39 | |
| Contraception | ||||||||
| None used | 55.67±19.99 | 53.46±22.62 | 47.53±25.53 | 47.14±18.08 | 202.46±73.92 | 25 (41.67) | 7 (11.67) | |
| Used | 58.98±18.14 | 51.65±17.80 | 53.15±19.50 | 50.59±17.52 | 215.34±61.46 | 26 (41.33) | 15 (25) | |
| P-value | 0.50 | 0.73 | 0.33 | 0.45 | 0.46 | 0.73 | 0.10 | |
| Condom usage | ||||||||
| Absent | 55.1±20.34 | 52.27±22.06 | 46.87±24.15 | 46.9±18.33 | 200.2±73.30 | 34 (56.67) | 14 (23.33) | |
| Present | 62.1±15.15 | 52.95±15.75 | 57.85±17.03 | 53.15±16.07 | 227.6±50.07 | 14 (23.33) | 8 (13.33) | |
| P-value | 0.17 | 0.9 | 0.07 | 0.20 | 0.13 | 1.00 | 0.77 | |
WHO: World Health Organization, QOL: Quality of life, FSFI: Female sexual function index, STI: Sexually transmitted infection, RTI: Reproductive tract infection, SD: Standard deviation, WHOQOL-BREF: World health organization quality of life brief version
DISCUSSION
STIs/RTIs can significantly impair both physical and emotional well-being by diminishing the QOL of women, causing discomfort, pain and significant fertility issues. Approximately 374 million new cases (1 of 4 STIs: Chlamydia [129 million], gonorrhoea [82 million], syphilis [7.1 million] and trichomoniasis [156 million]) of STIs occur every year according to the WHO (2023) data.[6] About 6% of adult Indian population is suffering from RTIs including STIs according to community-based survey from India. As per the National Acquired Immunodeficiency Syndrome Control Organization (2014), about 30–35 million episodes of STIs/ RTIs occur every year in our country.[7] QOL measures give a more direct measure of the impact of the disease on daily life and, this is more relevant in RTI/STIs where the condition is distressing physically and psychologically and treatment seeking is hindered by numerous factors.[8]
WHO-QOL-BREF questionnaire has been developed by the WHO for the assessment of QOL amongst patients belonging to different countries and cultures. On evaluation of the WHO-QOL-BREF scores, the scores were lowest in the environmental domain, followed by the second lowest in the social domain. In a study conducted by Valsangkar et al.,[8] all domains of QOL (measured by WHO-QOL-BREF questionnaire) were affected in the STIs/RTIs group, similar to our study. However, the largest impact of this study was on the social and sexual domains.
According to a study by Raj et al.,[2] the total health-related QOL (HRQOL) scores (mean ± SD) were 280.1 ± 83.56 (amongst controls), 196.9 ± 72.41 (genital human papillomavirus [HPV]), 141.0 ± 50.50 (herpes simplex virus [HSV]-2) and 103.4 ± 47.23 (mixed infection group). This was also the case in our study, where women with mixed infections (genital herpes and genital molluscum contagiosum) were the lowest scorers and the highest scorers were the women infected with genital molluscum contagiosum, followed by genital warts. Mean HRQOL scores were lowest in the physical and psychological domains in this study whereas in our study, the maximum impact was seen in the other two domains that is, social and environmental. Moreover, it suggests that STIs/RTIs in one way or the other can affect every domain of the QOL, either of directly or indirectly. In a study conducted by BarnackTavlaris et al.,[9] women with genital herpes reported low levels of QOL, similar to our study and there was evidence that herpes can negatively influence psychological well-being. Similarly in a study conducted by Taboulet et al.[10] on genital herpes, 23% patients reported feelings of depression, shame and/or lack of affection and 54% reported decreased sexual enjoyment. Moreover, this was observed in our study also as we found that the lowest psychological domain score belonged to herpes genitalis group, with a score of 36.13 ± 14.58, even lower than that of mixed infection group. The reason behind this could be attributed due to chronicity and recurrent nature of the disease, thereby causing a significant psychological impact.
A study on anogenital warts by Vilata et al.[11] revealed that these also lead to psychological distress, thereby diminishing the QOL. Woodhall et al.[12] reported similar results in their research. It is well recognised that much of the morbidity associated with genital warts is believed to be psychological.[13] In our study also, the individual domain scores as well as the total WHO-QOL-BREF score of genital warts were lower than the controls.
Candidal vulvovaginitis can also become chronic and frequently recurs, leading to significant psychological comorbidity and impacting QOL in a manner similar to herpes genitalis and genital warts. Nyirjesy et al.[14] observed that a proportion of 29 % patients who were suffering from candidal vulvovaginitis also had clinical depression. On the contrary in our study, women with candidal vulvovaginitis scored the second highest in psychological domain, only after women with genital warts.
However, they scored the third lowest in terms of the social domain score, with only women with mixed infection and herpes genitalis lower than them. The overall QOL score in these women was found to be 208.50 ± 70.29.
According to the WHO, sexual dysfunction is a significant public health issue that warrants regular investigation, as it has a profound impact on the QOL for both women and their partners. Landmark studies by Kinsey et al.[15] and Laumann et al.[16] brought the lens of scientific rigor to the subject of sexual health. These concerns have primarily been explored in relation to infections such as HPV and HSV. Ma et al.[17] utilised the Chinese version of the FSFI to assess sexual dysfunction and found that women with non-malignant cervical diseases exhibited a significantly higher prevalence of female sexual dysfunction (51.8% vs. 34.8%), along with lower scores for desire (43.2% vs. 26.3%), arousal (41.6% vs. 28.3%) and lubrication (51.2% vs. 36.9%) compared to the control group. Similar results were obtained in our study.
In a study conducted by Cai et al.[18] to assess the sexual QOL in young sexually active women suffering from genital Chlamydia trachomatis infection, reduced sexual QOL was reported in these women, indicated by lower FSFI scores for sexual desire (3.1 ± 1.1), lubrication (2.7 ± 1.2) and overall sexual function (21.3 ± 1.2). Even we found lower scores in our non-gonococcal cervicitis patients, with sexual desire and overall sexual function scores being 2.867 ± 1.63 and 20.600 ± 5.18, respectively. Lubrication scores were raised in our study, with a mean score of 4.311 ±.72. Moreover, women with non-gonococcal cervicitis were found to have the second highest score in the pain domain with a mean of 3.689 ± 1.59, only behind women with genital warts.
Giraldo et al.[19] studied the FSFI scores of 58 women assigned to three groups (recurrent vulvovaginal candidiasis (RVVC), localised provoked vulvodynia and control group) and found that lower FSFI scores were present in the study groups as compared to the control group; and lower scores for all domains except for desire were present in the candidiasis group as compared to the control group. We also found that patients with candidal vulvovaginitis had lower scores in all domains along with reduction in the mean score of overall sexual function as compared to the controls. Even amongst different STIs, women with candidal vulvovaginitis were found to have third lowest scores after women with mixed infection and herpes genitalis, in terms of sexual desire, arousal, lubrication, satisfaction, pain and overall sexual function domains. Moreover, they had the second lowest score in the orgasm domain only after women with herpes genitalis. The discordance between the two studies can be explained by the fact that women with herpes genitalis were not included in the previous study. The constant presence of genital infection or potential difficulties with movement of the pelvic floor muscles may interfere with the orgasmic capacity of these women.[20]
CONCLUSION
As QOL and sexual function, overall and in individual domains are adversely affected in women having STIs/ RTIs, it should be given significant importance in patient management since impairment in these areas is a cause of great distress in these women. As our study was hospital based with a limited sample size, further research with a larger community-based cohort is needed to validate our findings. This would support the use of QOL measures (WHO-QOL-BREF) and sexual function assessments (FSFI) in evaluating various treatment options for chronic and recurrent STIs/RTIs.
Ethical approval:
The research/study was approved by the Institutional Review Board at Lady Hardinge Medical College and Hospitals, number LHMC/ECHR/2014/518, dated October 30, 2014.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Global Epidemiology of Sexually Transmitted Diseases. Asian J Androl. 2008;10:110-4.
- [CrossRef] [PubMed] [Google Scholar]
- Health-related Quality of Life in Indian Patients with Three Viral Sexually Transmitted Infections: Herpes Simplex Virus-2, Genital Human Papilloma Virus and HIV. Sex Transm Infect. 2011;87:216-20.
- [CrossRef] [PubMed] [Google Scholar]
- Recurrent Genital Herpes Treatments and their Impact on Quality of Life. Pharmacoeconomics. 2003;21:853-63.
- [CrossRef] [PubMed] [Google Scholar]
- Development of the World Health Organization WHOQOL-BREF Quality of Life Assessment. The WHOQOL Group. Psychol Med. 1998;28:551-8.
- [CrossRef] [PubMed] [Google Scholar]
- The Female Sexual Function Index (FSFI): A Multidimensional Self-report Instrument for the Assessment of Female Sexual Function. J Sex Marital Ther. 2000;26:191-208.
- [CrossRef] [PubMed] [Google Scholar]
- Sexually Transmitted Infections (STIs) Available from: https://www.who.int/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis) [Last accessed on 2023 Nov 15]
- [Google Scholar]
- National AIDS Control Organization. MoHFW, GoI. Available from: https://naco.gov.in/sti-rti-services [Last accessed on 2023 Oct 10]
- [Google Scholar]
- Impairment of Quality of Life in Symptomatic Reproductive Tract Infection and Sexually Transmitted Infection. J Reprod Infertil. 2014;15:87-93.
- [Google Scholar]
- Psychological Adjustment among Women Living with Genital Herpes. J Health Psychol. 2011;16:12-21.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of Life and Use of Health Care among People with Genital Herpes in France. Acta Derm Venereol. 1999;79:380-4.
- [CrossRef] [PubMed] [Google Scholar]
- Validation and Clinical Use of the CECA, A Disease-specific Quality of Life Questionnaire for Patients with Anogenital Condylomata Acuminata. Acta Derm Venereol. 2008;88:257-62.
- [Google Scholar]
- Estimation of the Impact of Genital Warts On Health-related Quality of Life. Sex Transm Infect. 2008;84:161-6.
- [CrossRef] [PubMed] [Google Scholar]
- An International Survey of Patients with Genital Warts: Perceptions Regarding Treatment and Impact On Lifestyle. Int J STD AIDS. 1998;9:571-8.
- [CrossRef] [PubMed] [Google Scholar]
- Causes of Chronic Vaginitis: Analysis of A Prospective Database of Affected Women. Obstet Gynecol. 2006;108:1185-91.
- [CrossRef] [PubMed] [Google Scholar]
- Sexual Behavior Human Male. (1st ed). Canada: AbeBooks; Available from: https://www.abebooks.com/book-search/title/sexual-behavior-human-male/author/alfred-ckinsey/first-editi on [Last accessed on 2023 Oct 11]
- [Google Scholar]
- The Social Organization of Sexuality: Sexual Practices in the United States. 2000. Chicago, IL: University of Chicago Press; :750. Available from: https://press.uchicago.edu/ucp/books/book/chicago/S/bo3626005.html [Last accessed on 2023 Oct 11]
- [Google Scholar]
- Female Sexual Dysfunction in Women with Non-malignant Cervical Diseases: A Study from an Urban Chinese Sample. PLoS One. 2015;10:e0141004.
- [CrossRef] [PubMed] [Google Scholar]
- Genital Chlamydia Trachomatis Infection is Related to Poor Sexual Quality of Life in Young Sexually Active Women. J Sex Med. 2011;8:1131-7.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of Sexual Function in Brazilian Women with Recurrent Vulvovaginal Candidiasis and Localized Provoked Vulvodynia. J Sex Med. 2012;9:805-11.
- [CrossRef] [PubMed] [Google Scholar]
- Female Sexual Dysfunction. Psychiatr Clin North Am. 2010;33:323-38.
- [CrossRef] [PubMed] [Google Scholar]







