Translate this page into:
Parry–Romberg Syndrome Associated with Hypothyroidism
*Corresponding author: Shivani, Department of Dermatology, Indira Gandhi Institute of Medical Sciences, Patna, Bihar, India. drshivani4847@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shivani, Jaykar KC, Ganguly S, Pallavi UK, Kumar D. Parry–Romberg Syndrome Associated with Hypothyroidism. Indian J Postgrad Dermatol. doi: 10.25259/IJPGD_50_2025
Abstract
Parry–Romberg syndrome (PRS) is a rare degenerative disorder of unknown cause, marked by progressive unilateral facial atrophy. It predominantly affects females and commonly involves the left side of the face. We report a rare case of PRS in a 14-year-old male patient involving hemiatrophy of the right side of face involving skin, subcutaneous tissue, muscles of mastication, parotid gland, right hemimandible and maxilla. There was no family history of any syndromic disorder. In our case, the condition was associated with hypothyroidism, highlighting the need for further research to investigate a potential association between PRS and hypothyroidism.
Keywords
Hypothyroidism
Parry–Romberg syndrome
Progressive hemifacial atrophy
INTRODUCTION
Parry–Romberg syndrome (PRS) is a rare, acquired, slowly progressive typically unilateral hemifacial atrophy of skin, subcutaneous tissue, fat, muscles and osteocartilaginous structure commonly affecting dermatomes of trigeminal nerve.[1]
CASE REPORT
A 14-year-old male presented with the right-sided facial asymmetry, progressively worsening since age 7 [Figure 1]. He had a history of trauma at 6 years old, followed by gradual facial atrophy. His medical and family history was unremarkable.

- A 14-year-old male of Parry– Romberg Syndrome with the right hemifacial atrophy.
The physical examination revealed severe atrophy of skin and subcutaneous tissue along with areas of hyperpigmentation of the periorbital, maxillary and mandibular region of right face creating a sunken appearance. Neck palpation revealed a soft, non-tender goitre in anterior region. Lips and nose were deviated towards right side of face and enophthalmos of the right eye was present. Intraoral examination revealed atrophy of tongue papillae of the right side with multiple fissures. The right maxillary arch displayed dental crowding. No speech or hearing impairments were detected. Intellectual development was normal. There were no neurological symptoms. Hemogram, urinary analyses and antinuclear antibodies (ANAs) were within normal limits. Serum thyroid-stimulating hormone (TSH) was elevated (15 mIU/mL), free T4 was low (0.5 ng/dL) and anti-thyroid peroxidase (anti-TPO) antibodies were negative, indicating hypothyroidism. Electroencephalogram and electrocardiogram were normal. Histopathological examination showed atrophy of the epidermis, dermal sclerosis and atrophy of skin appendages, accompanied by a mild lymphocytic infiltrate [Figure 2].
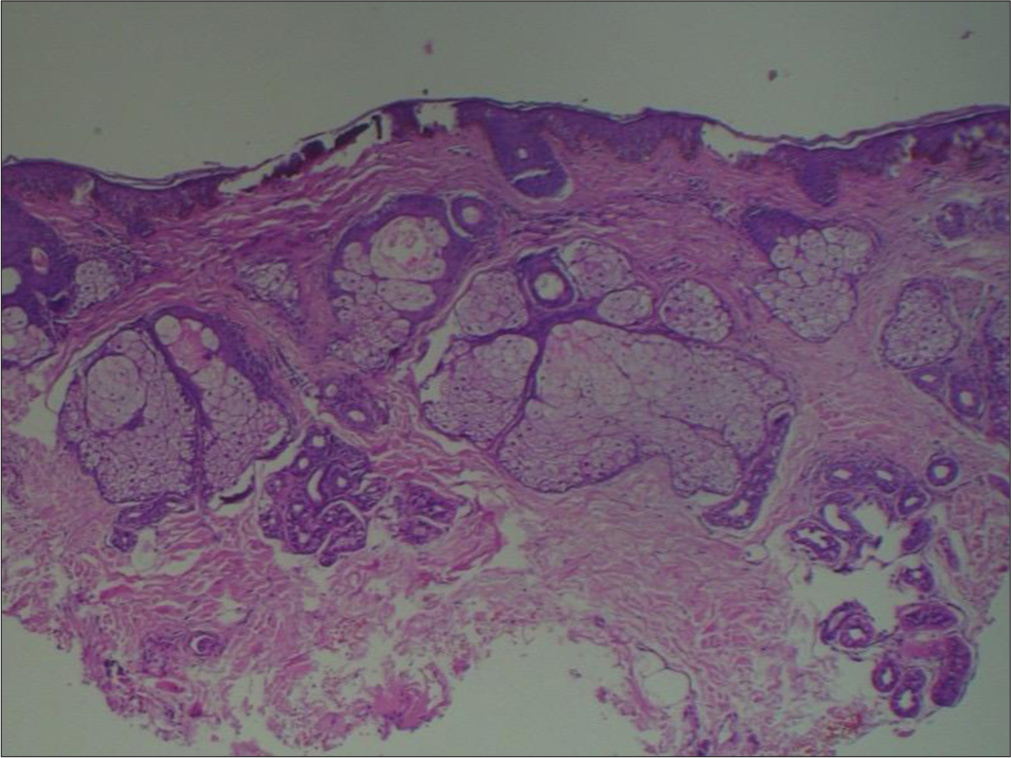
- Histopathology showing mild epidermal atrophy. Dense, hyalinised collagen bundles in the dermis with sparse superficial perivascular and periappendageal lymphohistiocytic infiltrate with atrophic adnexal structure. Subcutaneous extension of sclerosis is present at the base of section (Haematoxylin and Eosin,100X).
Computed tomography scan of head and face showed diffuse atrophy of right facial structures involving skin subcutaneous tissue, muscles of mastication, parotid gland, right hemimandible and maxilla with no intracranial lesion [Figure 3]. A diagnosis of Parry–Romberg syndrome (PRS) was made based on clinical, histopathological and radiological findings. Oral prednisone 1 mg/kg/day (tapered over 3 months) and methotrexate 15 mg/week with folic acid and levothyroxine 75 mcg/day were prescribed with regular follow-up. After 3 months of therapy, the patient did not show any progression in symptoms, skin texture became slightly smoother and the patient became biochemically euthyroid. He was kept on follow-up to ensure disease stabilisation before further planning reconstructive procedures for facial defects.

- 3D-computed tomography (a) face and (b-d) Non-contrast computed tomography head-neck demonstrating right hemifacial atrophy of soft-tissue and osseous structures; however, brain parenchyma appears normal.
DISCUSSION
PRS was first reported by Caleb Parry (1825) and then described by Moritz Romberg (1846).[1] Eulenberg (1871) coined the term progressive hemifacial atrophy. Stone reported an incidence of 1:700,000.[2] The female-to-male ratio is 3:1. The onset is insidious and usually presents in the first two decades of life but late onset has also been reported. Atrophy usually involves the left side of face. The etiopathogenesis still remains unclear but various theories including lymphocytic neurovasculitis, exogenous trauma, autoimmunity, endocrine disturbances, sympathetic dysregulation and infections have been suggested.[1] It was hypothesised that a history of trauma was present in 24–34% of PRS patients.[2]
PRS may coexist with other autoimmune disorders, including autoimmune thyroid diseases such as Hashimoto’s thyroiditis and Graves’ disease.[3,4] Recognition of this association is important, as thyroid dysfunction can significantly affect the clinical course and management of these patients.
In a case reported by Claudy et al.,(1992) occurrence of facial hemiatrophy and homolateral cervical band of scleroderma, complicated by hypothyroidism was described.[3] In a case reported by Lee et al, (2017) a 41-year-old woman diagnosed with PRS presented with Hashimoto’s thyroiditis-induced hypothyroidism, evidenced by elevated TSH, low free T4 and positive ANAs.[4] Notably, this was the first documented case in Korean ophthalmologic literature where PRS coexisted with hypothyroidism, suggesting a potential but rare autoimmune overlap.[4]
In our case, the patient also presented with hypothyroidism, indicated by elevated serum TSH, low free T4 and negative anti-TPO antibodies, possibly suggesting seronegative autoimmune thyroiditis. However, due to the limited number of reported cases and lack of studies, a causal relationship remains speculative. Proposed theories suggest that both conditions may arise from a common autoimmune response directed against distinct tissues, or from a genetic predisposition that increases susceptibility to both disorders.[1,3,4]
Therefore, it is imperative that clinicians consider screening for thyroid function in patients diagnosed with PRS, especially when systemic signs are present. Further studies with larger cohorts are warranted to explore whether thyroid dysfunction in PRS is an incidental finding or part of a broader autoimmune spectrum.
PRS is associated with various extracutaneous manifestations, with neurological complications being the most common.[1,2] Ocular issues such as enophthalmos, uveitis and restrictive strabismus, along with neurological conditions such as seizures, headaches and cranial neuropathies, have been reported. Oral anomalies, including dental malformations and delayed tooth eruption, are also described.
Historically, there has been debate over whether PRS is a variant of linear scleroderma, known as morphea en coup de sabre (ECDS) or a distinct condition. Duymaz et al. proposed that PRS presents as unilateral facial atrophy without prior induration or inflammation, whereas ECDS manifests as unilateral, band-like sclerosis in the frontoparietal region with associated induration.[5] Tollefson and Witman suggested that PRS and ECDS often coexist and may be subtypes of craniofacial localised scleroderma.[6]
The differential diagnosis of PRS includes other forms of localised scleroderma, Rasmussen encephalitis, Barraquer– Simons syndrome and bulbar poliomyelitis.[1] There is no definite treatment available for PRS. Treatment aims to halt disease progression with medical therapy followed by cosmetic surgeries. Corticosteroids and immunosuppressant therapy are typically used to treat the active stage of the disease.
This case is being reported because very few cases of association of PRS with thyroid disease have been described in literature. Early diagnosis and multidisciplinary treatment are crucial for managing PRS and mitigating its aesthetic, functional and psychological impact.
CONCLUSION
This case draws attention to a rare but important association between Parry-Romberg Syndrome and hypothyroidism. Although a definitive causal relationship remains unproven, their coexistence may suggest an underlying autoimmune connection or genetic predisposition. Given the potential impact of thyroid dysfunction on disease progression and management, routine thyroid screening should be considered in patients with PRS, especially when systemic signs are present. Given the complex and multisystem nature of PRS, early detection and a coordinated, multidisciplinary approach to management are essential. Further research with larger patient cohorts is warranted to better understand the pathophysiological link and to guide further treatment strategies.
Ethical approval:
Institutional Review Board approval is not required.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Collections from the Unpublished Medical Writings of the Late Caleb Hillier Parry Gaffney: Underwoods; 1825. p. :592.
- [Google Scholar]
- Hemiatrophia Facialis Progressiva In: Lehrbuch der Funktionellen Nervenkrankheiten auf Physiologischer Basis. Berlin: Verlag von August Hirschwald; 1871. p. :712-26.
- [Google Scholar]
- Facial hemiatrophy, homolateral cervical band-like scleroderma, and thyroid disease. Annales de Dermatologie et de Vénéréologie. 1992;119:543-545.
- [Google Scholar]
- Parry-Romberg Syndrome Associated with Hypothyroidism. J Korean Ophthalmol Soc. 2017;58:857-61.
- [CrossRef] [Google Scholar]
- Parry-Romberg Syndrome: Facial Atrophy and its Relationship with Other Regions of the Body. Ann Plast Surg. 2009;63:457-61.
- [CrossRef] [PubMed] [Google Scholar]
- En Coup de Sabre Morphea and Parry-Romberg Syndrome: A Retrospective Review of 54 Patients. J Am Acad Dermatol. 2007;56:257-63.
- [CrossRef] [PubMed] [Google Scholar]







