Translate this page into:
Neonatal Staphylococcal Scalded Skin Syndrome - “Scary but Safe”
*Corresponding author: Rajesh Rajagopalan, Department of Dermatology, Venereology and Leprology, Government Erode Medical College Hospital, Perundurai, Erode, Tamil Nadu, India. rajeshderma@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sundareswaran D, Rajagopalan R, Vethanayagam M, Kandasamy R, Karattupalayam Govindan S, Bhavani Rajendran B. Neonatal Staphylococcal Scalded Skin Syndrome - “Scary but Safe”. Indian J Postgrad Dermatol. doi: 10.25259/IJPGD_181_2024
Dear Editor,
Staphylococcal Scalded Skin Syndrome (SSSS) also called Ritter’s disease is a rare and potentially life-threatening condition characterised by widespread exfoliation of the skin, primarily affecting infants and young children caused by Staphylococcus aureus strains producing exfoliative toxins (ET- A and B). ETs target the cell adhesion protein desmoglein-1 leading to the separation of keratinocytes just beneath the granular layer in the epidermis. Community-acquired methicillin-resistant Staphylococcus aureus (MRSA) is commonly implicated in SSSS in neonates.
A 12-day-old female neonate[1-5] was referred from a secondary care hospital to our facility with complaints of peeling skin, pus-filled skin lesions all over the body and fever persisting for the past 10 days. The mother of the baby, a teenager and migrant, had an unimmunised pregnancy and delivered the baby while working on a farm. At the time of admission, the neonate presented with irritability, fever, tachycardia and multiple erythematous papules, pustules, bullae and erosions distributed across various body regions.
Clinical examination revealed positive Nikolsky’s sign [Figure 1], indicative of epidermal detachment upon slight pressure. Blood and pus cultures were obtained, with the latter showing heavy growth of S. aureus sensitive to several antibiotics. Gram staining of pus revealed Gram-positive cocci in pairs and tetrads. These findings confirmed the diagnosis of SSSS. The neonate received intravenous vancomycin for 7 days and topical mupirocin for localised lesions. Barrier nursing and strict infection control measures were implemented.
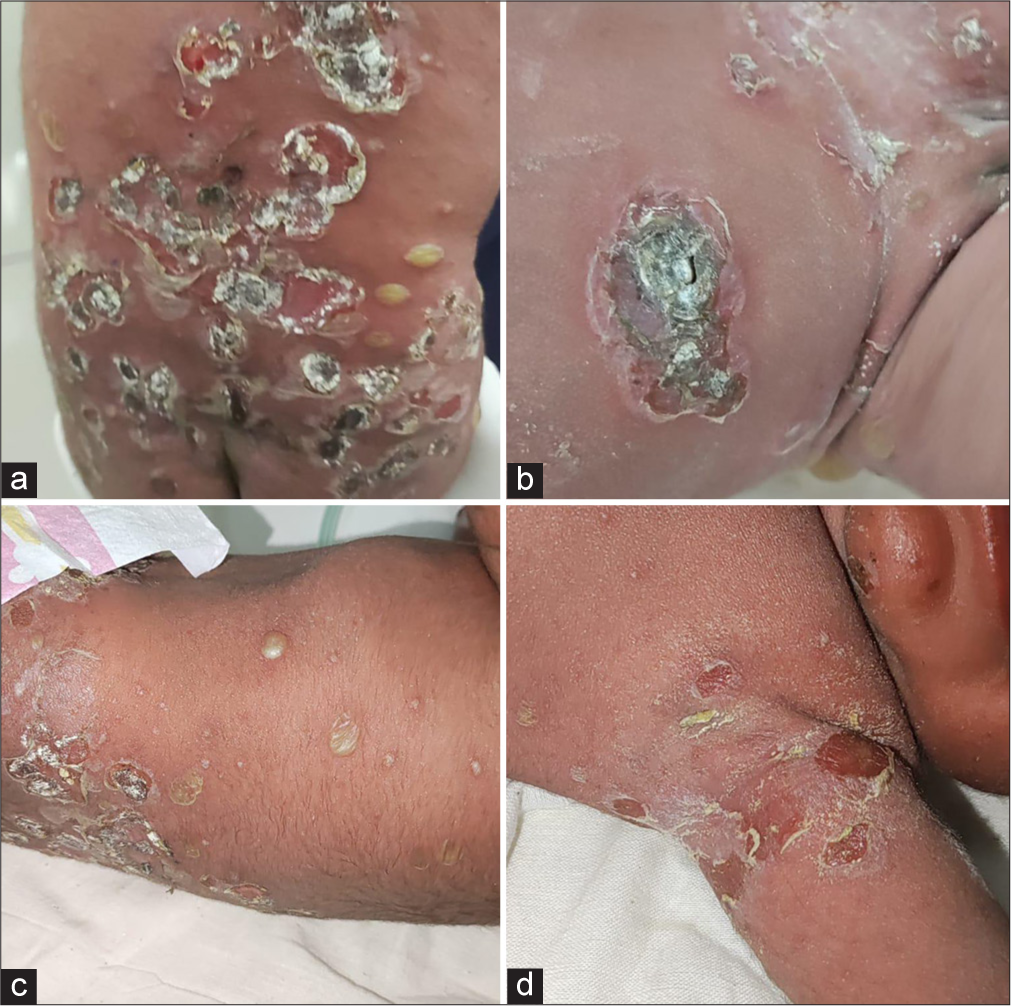
- At the time of admission - Multiple well defined erythematous papules, pustules, bullae and erosions with crusting present over (a) back, (b) periumbilical region, (c) lateral aspect of chest and abdomen and (d) left axilla.
Over the course of treatment, the baby responded well, with the resolution of skin lesions and improvement in clinical parameters. Vitals were monitored closely, and the neonate was shifted from the neonatal intensive care unit to the mother’s side just after 3 days. Upon discharge, the skin lesions had completely resolved, with minimal post-inflammatory changes observed.
Other differential diagnoses were also considered as follows. In bullous impetigo, the ETs [Figure 2] remain local in the infected skin but in SSSS, the ETs are spread haematogenously resulting in widespread skin involvement. Absence of mucosal involvement as seen in SSSS, positive Nikolsky’s sign and characteristic Gram-positive cocci in cultures helps in diagnosis.[2]
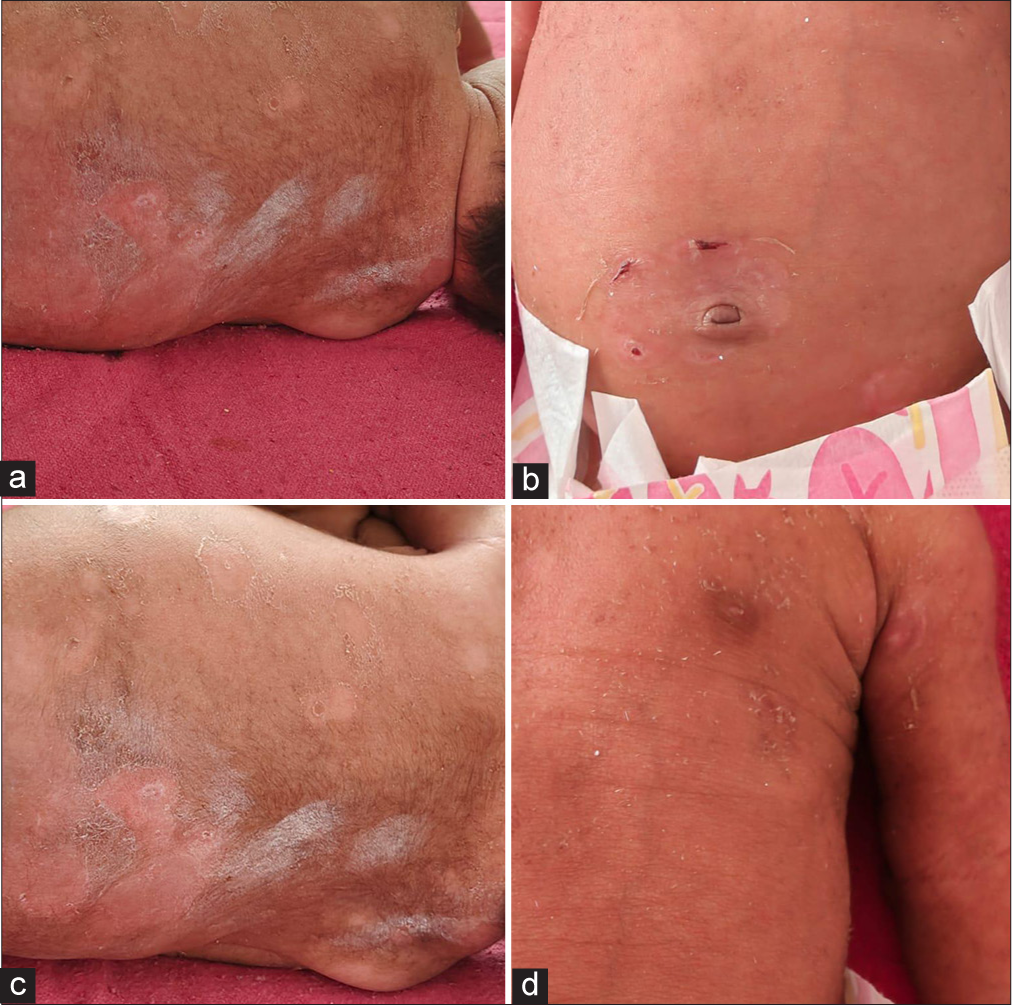
- Day 7 after treatment - all erosions resolved completely. All lesions over the (a) back, (b) periumbilical region, (c) lateral aspect of chest and abdomen and (d) left axilla healed completely.
Toxic epidermal necrolysis is often triggered by medications or infections. Diagnosis is clinical, based on the characteristic presentation of widespread epidermal detachment. Treatment involves immediate discontinuation of the offending medication, supportive care and immunosuppressive therapy.
Epidermolysis bullosa is a group of genetic disorders characterised by fragile skin that forms blisters and erosions in response to minor trauma or friction caused by mutations in genes encoding for proteins such as anchoring fibrils, hemidesmosomes and keratin. Chronic wounds, scarring and deformities occur. Diagnosis is based on clinical presentation, family history, and skin biopsy shows separation of the epidermis from the underlying dermis. Treatment focuses on wound care, including gentle non-adherent dressings, and prevention of infection, pain management and nutritional support.
Neonatal pemphigus is rare, caused by the transfer of maternal autoantibodies across the placenta to the foetus, resulting in blistering and erosions of the skin and mucous membranes and presents shortly after birth with flaccid blisters and erosions on the skin and mucous membranes. Lesions heal without scarring once the maternal autoantibodies are cleared from the infant’s circulation. Diagnosis is suspected based on clinical presentation and confirmed through immunofluorescence studies demonstrating the presence of maternal autoantibodies in the infant’s skin biopsy. Treatment includes plasmapheresis or immunoglobulin therapy and topical corticosteroids.
Management of SSSS involves a multidisciplinary approach, including supportive care, antibiotic therapy targeting S. aureus and infection control measures.[3,4] The first line of management is anti-staphylococcal penicillins such as flucloxacillin, dicloxacillin, cefazolin, clindamycin and daptomycin. The second line of management is vancomycin (when MRSA is suspected), linezolid and tigecycline.
Topical agents like mupirocin can be used for localised lesions. Strict infection control practices, including barrier nursing and hand hygiene, are essential to prevent spread.
SSSS is a rare but serious condition that requires prompt recognition and appropriate management. This case highlights the importance of a thorough clinical evaluation in suspected cases. Early initiation of effective antibiotic therapy and supportive care can lead to favourable outcomes and prevent potential complications. Children usually recover in 7 days with early administration of appropriate antibiotics. Mortality in children is 4% and in adults, it is comparatively very high as 60%.[5] Continued vigilance and adherence to infection control protocols are essential in managing SSSS and reducing its morbidity and mortality rates.
Ethical approval:
Institutional Review Board approval is not required.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Staphylococcal Scalded Skin Syndrome In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/nbk448135 [Last accessed on 2023 Jul 25]
- [Google Scholar]
- Staphylococcal Scalded Skin Syndrome in Child. A Case Report and a Review from Literature. J Crit Care Med (Targu Mures). 2016;2:192-7.
- [CrossRef] [PubMed] [Google Scholar]
- Staphylococcal Scalded Skin Syndrome in a 4-Year-Old Child: A Case Report. J Med Case Rep. 2018;12:20.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical, Microbial, and Biochemical Aspects of the Exfoliative Toxins Causing Staphylococcal Scalded-Skin Syndrome. Clin Microbiol Rev. 1999;12:224-42.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiological Data of Staphylococcal Scalded Skin Syndrome in France from 1997 to 2007 and Microbiological Characteristics of Staphylococcus aureus Associated Strains. Clin Microbiol Infect. 2012;18:E514-21.
- [CrossRef] [PubMed] [Google Scholar]






