Translate this page into:
Nailfold Capillaroscopy in Psoriatic Patients with Metabolic Syndrome: A Comparative Observational Study
*Corresponding author: Vineet Relhan, Department of Dermatology, Fortis Hospital, Greater Noida, Uttar Pradesh, India. vineetrelhan@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Pal V, Relhan V. Nailfold Capillaroscopy in Psoriatic Patients with Metabolic Syndrome: A Comparative Observational Study. Indian J Postgrad Dermatol. 2025;3:1-6. doi: 10.25259/IJPGD_82_2024
Abstract
Objectives:
Psoriasis, a systemic disorder, is linked with metabolic comorbidities. Nailfold capillaroscopy (NFC), a non-invasive technique, is utilised to evaluate microcirculation in the nailfold area. This study aimed at assessing nailfold capillary changes among psoriatic patients with metabolic syndrome (MeS) and compared these finding to those of healthy controls.
Materials and Methods:
An evaluation of 75 patients with psoriasis and 75 age- and sex-matched healthy controls were done. NFC was performed using universal serial bus videodermatoscope on the 4th and 5th digits of both hand and MeS was diagnosed using National Cholesterol Education Program and Adult Treatment Panel III criteria.
Results:
Twenty-five (33%) psoriatic patients and 10 (13.3%) healthy control had MeS (P = 0.004). The mean nailfold capillary density in psoriasis patients with and without MeS was significantly less than that in healthy controls (P < 0.005 and <0.001, respectively). Dilated, bushy and dropout capillaries were significantly higher in Psoriatic patients with MeS; whereas, meandering, dilated, giant, bushy, bizarre capillaries, microhaemorrhages, dropouts and avascular areas were significantly higher in psoriatic patients without MeS when compared to respective groups of healthy control with MeS or without MeS.
Conclusion:
Decreased mean capillary density and higher incidence of budding and bushy capillaries in psoriatic patients with MeS as compared to psoriatic patients without MeS points toward a pathogenic role of MeS in microvascular damage; however, the absence of an association with disease duration and severity suggests that these capillary changes might serve as early markers of MeS, which warrants further investigation in larger and prospective studies.
Keywords
Metabolic syndrome
Nailfold capillaroscopy
Psoriasis
INTRODUCTION
Psoriasis is an inflammatory disorder affecting 0.84% of the global population.[1] Psoriasis is a systemic disease associated with metabolic, psychological, arthritic and cardiovascular comorbidities.[2,3] Psoriasis is a prototypical T helper type 1 (Th1) inflammatory disorder characterised by increased levels of Th-1 cytokines, intracellular adhesion molecule, E-selectin, angiogenic factors and vascular endothelial growth factor. These inflammatory mediators affect angiogenesis, lipid metabolism, insulin signalling, adipogenesis and epidermal proliferation, leads to microvascular changes in psoriasis, which can precede the skin manifestations and may resolve with treatment.[4,5] These mediators are also crucial for the development of metabolic syndrome (MeS), which explains the presence of microvascular changes in MeS.[4] MeS consists of hypertension (HTN), abdominal obesity, dyslipidaemia and glucose intolerance, which further elevate the likelihood of developing cardiovascular disease (CVD).[2] Microvascular changes in MeS can be assessed non-invasively using nailfold capillaroscopy (NFC).[5] Videocapillaroscope serves as a gold standard instrument for NFC; however, it’s cost often limits its availability in most clinical settings. On the other hand, universal serial bus (USB) videodermatoscope is a widely available and less expensive instrument.[6,7] Nailfold capillary changes in psoriasis include decreased capillary density, presence of avascular areas and increased number of morphologically abnormal capillaries.[8] NFC has become increasingly important for diagnosing rheumatic and connective tissue disease and can also be utilised to detect neovascular alterations associated with diabetes and HTN.[5] To the best of our knowledge, there is a paucity of literature assessing nailfold capillary changes among psoriatic patients with MeS.
MATERIALS AND METHODS
This comparative, observational study was conducted at the Department of Dermatology, University of Delhi, India, for a period of 1 year (March 2021–March 2022). Clinically diagnosed cases of psoriasis were enrolled by convenience sampling. Healthy volunteers from the Hospital staff (doctors, nurses and workers) were matched for age and sex before recruited as controls. A total of 150 participants with 75 psoriasis patients and 75 healthy controls were recruited. Pregnant and lactating females and patients of Raynaud’s phenomenon, paronychia, periungual traumatic lesions, smoker and connective tissue disorders were excluded from the study.
The psoriasis area and severity index (PASI) score was used to calculate disease severity and patients were categorised mild (PASI ≤3), moderate (PASI between 3 and 10) or severe (PASI ≥10).[9] National Cholesterol Education Program and Adult Treatment Panel III criteria was used to make the diagnosis of MeS.[10]
NFC was done at an ambient room temperature where the subject sits for 15–20 min and the hand resting on a dull, non-refractile surface at hearts level. The fourth and fifth digits of hand’s were used for the morphological observation due to maximum transparency of the skin in these fingers. Each finger was gently wiped with an alcohol swab and after 2–3 min, 1–2 drop of immersion oil was put on the proximal nailfold for better visualisation of the capillaries. NFC was carried out under the polarising mode of USB videodermatoscope (dinolite AM7515ZT). Cuticle near the proximal nailfold was marked using an ultra-thin marker and the images were clicked on both side of the marked point. The images were studied with the USB videodermatoscope calibration software and 2 mm distance on each side of marked point was used for counting the distal most capillary loop. A total of 4 mm length was used for the counting of capillaries. A total of 16 mm length was used in all four fingers for counting capillaries. Dividing the total number of capillaries by 16 yielded the mean nailfold capillary density. Images of capillaries were captured through USB videodermatoscope in jpg format, saved on a hard drive and analysed by two unbiased evaluators. Both quantitative (mean capillary density) and qualitative parameters (bushy, dilated, giant, bizarre, tortuous, meandering capillary, microhaemorrhage, avascular area and subpapillary venous plexus) were evaluated.[11-13]
Written informed consent was obtained from all the participants. The research protocol was approved by the Institutional Ethics Committee.
Statistical analysis
The collected data was entered in Microsoft Excel and analysed using the Statistical Package for social Sciences (SPSS) version 25. Quantitative data were expressed by mean, standard deviation and difference between two means were tested by student t test or Mann Whitney U test. Qualitative data were summarised in percentages and the difference between the proportions was analysed by Chi-square test or Fisher’s exact test. P < 0.05 indicates statistical significance.
RESULTS
Both the groups were age- and sex-matched. The duration of psoriasis ranged from as short as one month to as long as 40 years. The PASI score ranged from 0.3 to 52.7. Maximum number of cases 60 (80%) had psoriasis of <10 years. Five cases had at least one family member suffering from psoriasis. Among 75 cases, 13 (17.35%) cases had a history of comorbidities, six had diabetes mellitus (DM), five had HTN and two had both DM and HTN. All psoriatic patients with DM had MeS and three patients with HTN had MeS.
According to the National Cholesterol Education Program and Adult Treatment Panel III criteria, 25 (33.3%) psoriatic cases had MeS and 10 (13.3%) healthy controls had MeS. Cases had significantly more participants with MeS than controls (P = 0.004). Majority of the cases with MeS, 14 (18.67%) had moderate psoriasis followed by 8 (10.67%) of mild psoriasis and 3 (4%) of severe psoriasis.
Prevalence of MeS and its components (means ± standard deviation [SD]) among cases and control groups
Waist circumference among male participants was significantly higher in cases than in controls (90.58 ± 9.19 vs. 85.60 ± 5.96 P < 0.001) but non-significant among female participants. Serum triglyceride level and fasting blood sugar (FBS) level among cases was significantly higher than in controls (P = 0.032. and P < 0.001, respectively).
Comparison of components (mean ± SD) of MeS among cases and healthy control with MeS
Systolic blood pressure (BP) in cases was significantly higher than in controls (135.64 ± 13.57 vs. 124.70 ± 8.25 P = 0.038). High-density lipoprotein level in cases was significantly higher than in controls (43.72 ± 7.39 vs. 35.00 ± 7.89 P = 0.007). FBS level among cases was significantly higher than in controls (108.16 ± 33.70 vs. 101.10 ± 35.37 P = 0.048).
Comparison of NFC changes among cases and healthy control with MeS
Twenty-five psoriatic cases and 10 healthy controls had MeS. NFC density in cases was significantly lower than in controls (6.33 ± 0.63 vs. 7.16 ± 0.73 P = 0.005). Dilated capillaries and dropouts were significantly higher in psoriatic patients than that in controls. P = 0.02. Twelve (48.0%) participants in the psoriatic group had bushy capillaries. None of the controls had bushy capillaries and the association was statistically significant (P = 0.0072) [Figures 1-3]. Rest morphological parameters (Meandering, bizarre, giant, budding, criss-cross capillary and avascular area) were higher in psoriatic patients than in healthy controls. Tortuous capillaries and microhaemorrhages were higher in healthy control than in psoriatic patients but the association was not statistically significant [Table 1].
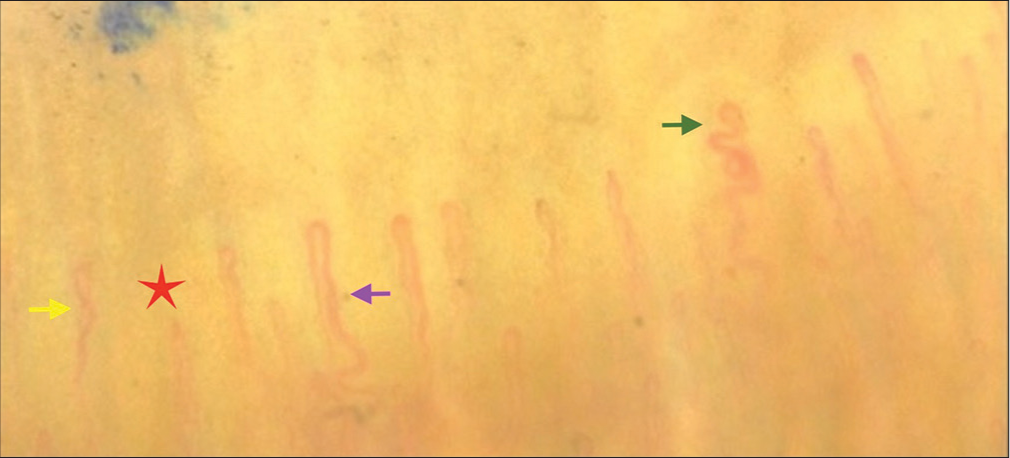
- Nailfold capillaroscopy of psoriatic patient with metabolic syndrome showing budding capillary (green arrow), dilated capillary (purple arrow), capillary drop-out (red star) and meandering capillary (yellow arrow).
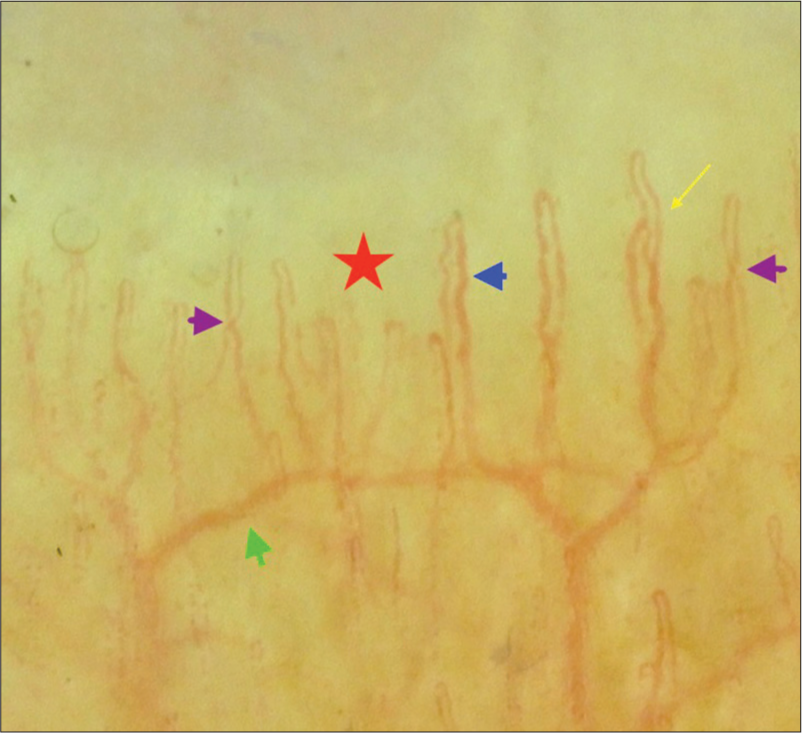
- Nailfold capillaroscopy of psoriatic patient with metabolic syndrome showing subpapillary venous plexus (green arrow), criss-cross capillary (purple arrows), avascular area (red star) ramified capillary (yellow arrow) and dilated capillary (blue arrow).

- Nailfold capillaroscopy of healthy control with metabolic syndrome showing dilated capillary (purple arrow), tortuous capillary (green arrow) and capillary dropout (red star).
| Parameters | Group | P-value | |
|---|---|---|---|
| Case (n=25) | Control (n=10) | ||
| Density (mean±SD) | 6.33±0.63 | 7.16±0.73 | 0.005 |
| Tortuous, n (%) | 8 (32.0) | 5 (50.0) | 0.444 |
| Meandering, n (%) | 13 (52.0) | 3 (30.0) | 0.285 |
| Dilated, n (%) | 13 (52.0) | 1 (10.0) | 0.028 |
| Giant, n (%) | 7 (28.0) | 0 (0.0) | 0.084 |
| Bushy, n (%) | 12 (48.0) | 0 (0.0) | 0.007 |
| Bizarre, n (%) | 5 (20.0) | 0 (0.0) | 0.292 |
| Microhaemorrhage, n (%) | 0 (0.0) | 1 (10.0) | 0.286 |
| Dropout, n (%) | 16 (64.0) | 2 (20.0) | 0.027 |
| Avascular area, n (%) | 8 (32.0) | 0 (0.0) | 0.073 |
| Subpapillary plexus, n (%) | 10 (40.0) | 0 (0.0) | 0.034 |
| Criss-cross, n (%) | 13 (52.0) | 5 (50.0) | 1.000 |
| Budding, n (%) | 6 (24.0) | 0 (0.0) | 0.152 |
SD: Standard deviation, NFC: Nailfold capillaroscopy
Comparison of NFC changes among cases and healthy control without MeS
Fifty cases and 65 healthy controls had no MeS. NFC density in cases was significantly lower than in controls (6.44 ± 0.5 vs. 7.27 ± 0.35 P < 0.001). Meandering, dilated, giant, bushy, bizarre capillaries, microhaemorrhages, dropouts and avascular areas were significantly higher in psoriatic patients without MeS than that in controls without MeS (P < 0.001). Psoriatic patients without MeS had significantly higher criss-cross, budding capillaries than healthy controls without MeS. Subpapillary venous plexus visibility was significantly higher in psoriatic patients 14 (28.0%) than in healthy control8 (12.3%) (P = 0.034) [Table 2 and Figure 4].
| Parameters | Group | P-value | |
|---|---|---|---|
| Case (n=50) | Control (n=65) | ||
| Density, mean±SD | 6.44±0.55 | 7.27±0.35 | <0.001 |
| Tortuous, n (%) | 22 (44.0) | 20 (30.8) | 0.144 |
| Meandering, n (%) | 25 (50.0) | 1 (1.5) | <0.001 |
| Dilated, n (%) | 26 (52.0) | 7 (10.8) | <0.001 |
| Giant, n (%) | 14 (28.0) | 0 (0.0) | <0.001 |
| Bushy, n (%) | 13 (26.0) | 1 (1.5) | <0.001 |
| Bizarre, n (%) | 18 (36.0) | 3 (4.6) | <0.001 |
| Microhaemorrhage, n (%) | 14 (28.0) | 0 (0.0) | <0.001 |
| Dropout, n (%) | 32 (64.0) | 9 (13.8) | <0.001 |
| Avascular area, n (%) | 22 (44.0) | 0 (0.0) | <0.001 |
| Subpapillary plexus, n (%) | 14 (28.0) | 8 (12.3) | 0.034 |
| Criss-cross, n (%) | 28 (56.0) | 17 (26.2) | 0.001 |
| Budding, n (%) | 6 (12.0) | 0 (0.0) | 0.006 |
SD: Standard deviation, NFC: Nailfold capillaroscopy
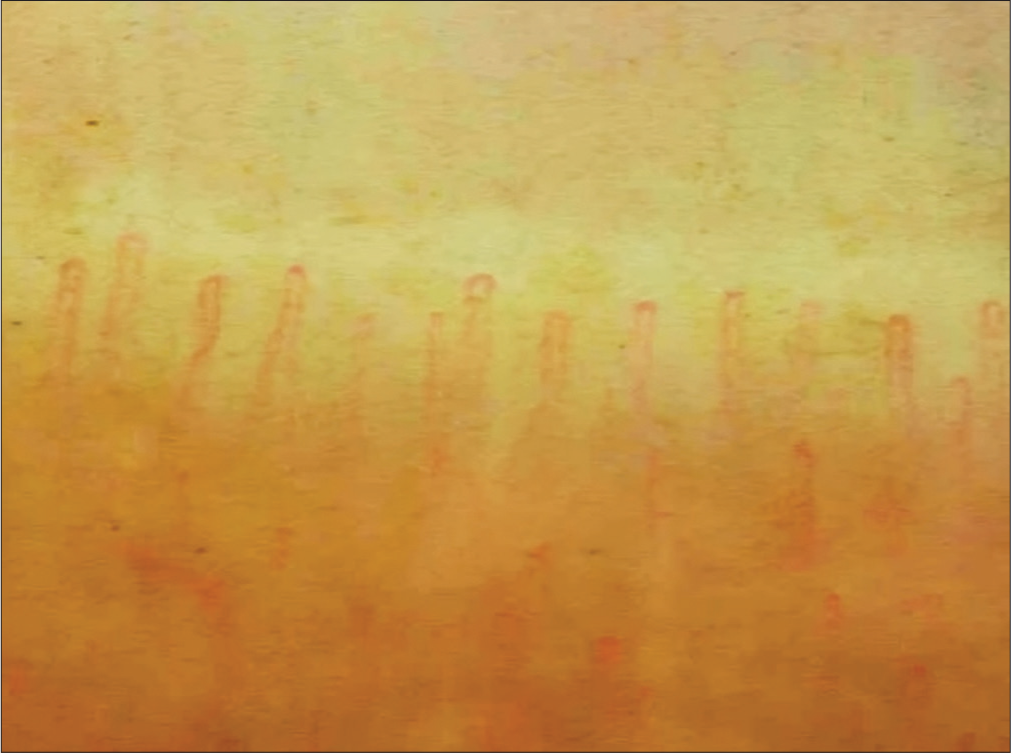
- Nailfold capillaroscopy of healthy control showing regular and parallel arrangement of nailfold capillary.
Comparison of NFC changes among psoriatic patients with and without MeS
Twenty-five psoriatic patients had MeS and 50 did not have MeS. The body surface area (BSA) and PASI score among both groups was non-significant (P = 0.74 and 0.61, respectively). Budding capillaries and Bushy capillaries were higher in psoriatic patients with MeS; however, microhaemorrhages were significantly higher in psoriatic patients without MeS. Dilated and giant capillaries were equal in both groups [Table 3].
| Parameter | Cases | P-value | |
|---|---|---|---|
| With MeS (n=25) | Without MeS (n=50) | ||
| Density (mean±SD) | 6.33±0.63 | 6.44±0.55 | 0.449 |
| Tortuous, n (%) | 8 (32.0) | 22 (44.0) | 0.317 |
| Meandering, n (%) | 13 (52.0) | 25 (50.0) | 0.870 |
| Dilated, n (%) | 13 (52.0) | 26 (52.0) | 1.000 |
| Giant, n (%) | 7 (28.0) | 14 (28.0) | 1.000 |
| Bushy, n (%) | 12 (48.0) | 13 (26.0) | 0.057 |
| Bizarre, n (%) | 5 (20.0) | 18 (36.0) | 0.157 |
| Microhaemorrhage, n (%) | 0 (0.0) | 14 (28.0) | 0.003 |
| Dropout, n (%) | 16 (64.0) | 32 (64.0) | 1.000 |
| Avascular area, n (%) | 8 (32.0) | 22 (44.0) | 0.317 |
| Subpapillary plexus, n (%) | 10 (40.0) | 14 (28.0) | 0.294 |
| Criss-cross, n (%) | 13 (52.0) | 28 (56.0) | 0.743 |
| Budding, n (%) | 6 (24.0) | 6 (12.0) | 0.198 |
SD: Standard deviation, NFC: Nailfold capillaroscopy, MeS: Metabolic syndrome
DISCUSSION
Psoriasis is a systemic inflammatory condition, which confers an increased risk of cardiovascular disorders. In our present study, a significant higher prevalence of MeS were found in psoriatic patients as compared to healthy controls. Same observations were also reported by Nisa and Qazi in 2010, they found that 28% of psoriatic patients and 6% of healthy controls had MeS.[14] Our study revealed that the disease severity was correlated with higher nailfold capillary changes but not correlated with a higher rate of MeS. Neimann et al., in 2006, recruited 1,27,706 psoriatic patients and found that the severity of the disease corelated with the higher rate of obesity and DM; however, HTN and hyperlipidaemia are not independently associated with severe disease.[15] A study by Kothiwala et al. found that the prevalence of MeS increased with increasing disease severity.[16] A study by Gisondi et al., in 2007, found no relationship between MeS prevalence and psoriasis severity.[17] Similarly, Fernández-Armenteros et al., in 2019, found no relation between psoriasis severity and MeS.[18] In our study, among each parameters of MeS systolic BP, obesity (Waist Circumference), triglycerides and FBS were significantly higher in psoriatic patients than in healthy controls, similar observations were reported by Kothiwala et al. in 2016.[16]
Psoriatic patients without MeS had significantly lower nailfold capillary density than that in controls without MeS. Psoriatic patients without MeS demonstrated significantly higher qualitative parameters (bushy, dilated, giant, bizarre and meandering capillary, microhaemorrhage, avascular area and subpapillary venous plexus visibility) compared to healthy controls without MeS.
Nailfold capillary density in patients of psoriasis with MeS was significantly less as compared to controls with MeS. Among qualitative parameters, dilated capillary, bushy capillary, capillary dropout and subpapillary venous plexus visibility were significantly higher in psoriasis with MeS than controls with MeS. These capillary morphologies suggest that neovascularisation is driven by tissue hypoxia and local generation of vascular growth factors which are due to vascular inflammation and atherosclerosis caused by psoriasis and MeS.[13,19] Numerous research has shown that psoriatic are strongly associated with cerebrocardiovascular diseases, depression, anxiety, osteoporosis, non-alcoholic fatty liver disease and end-stage renal disease; similarly, MeS is an independent contributor for CVDs.[19-23] The pathogenesis of psoriasis and MeS has overlapping genetic predisposition and inflammatory pathways and having both conditions, psoriasis and MeS, leads to an increased risk of CVD.[19,24] This ancillary inflammation in the capillary wall by MeS correlates with our NFC finding that bushy capillary, capillary dropout and visibility of subpapillary venous plexus were significantly higher in psoriatic patients with MeS than that in controls with MeS. NFC may enable us to quickly identify psoriatic patients who are at an increased risk of developing CVD.
A systematic review by Wu et al. showed that systemic treatment of psoriasis was associated with reduced vascular inflammation and cardiovascular events.[24] Adequate control of MeS through medication or lifestyle changes has a beneficial effect on psoriasis.[23] NFC has the potential to aid in early initiation of systemic treatment for psoriatic patients at risk of complications. NFC may further help us in the follow-up of these patients and their response to treatment.
Limitation
A less number of participants with MeS. An unequal distribution of participants with MeS in psoriatic as well as control groups and no follow-up of the patients to assess the effect of treatment on nailfold capillary changes are the major limitation of this study.
CONCLUSION
The prevalence of MeS was higher in psoriatic patients. The severity of psoriasis is not related to the development of MeS. MeS is associated with reduced nailfold capillary density and increases abnormal capillary morphologies in both psoriatic patients and healthy control groups. NFC may contribute to the early recognition of patients which require cardiovascular preventive measures, early initiation of systemic therapy, follow-up and response to treatment. Further, longitudinal study is required to establish temporal relationships between psoriasis, MeS and nailfold capillary changes.
Ethical approval
The research/study approved by the Institutional Review Board at Maulana Azad Medical College, number IEC/MAMC/82/10/2020/no.46, dated 28 December 2020.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Global Burden of Psoriasis-comparison of Regional and Global Epidemiology, 1990 to 2017. Int J Dermatol. 2020;59:566-71.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of Metabolic Syndrome in Chinese Psoriasis Patients: A Hospital-based Cross Sectional Study. J Diabetes Investig. 2018;9:39-43.
- [CrossRef] [PubMed] [Google Scholar]
- Metabolic Syndrome and Psoriatic Arthritis among Patients with Psoriasis Vulgaris: Quality of Life and Prevalence. J Dermatol. 2019;46:3-10.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriasis and Metabolic Disease: Epidemiology and Pathophysiology. Curr Opin Rheumatol. 2008;20:416-22.
- [CrossRef] [PubMed] [Google Scholar]
- Nailfold Capillaroscopy in Psoriasis. Med J Armed Forces India. 2021;77:75-81.
- [CrossRef] [PubMed] [Google Scholar]
- A Study Comparing Videocapillaroscopy and Dermoscopy in the Assessment of Nailfold Capillaries in Patients with Systemic Sclerosis-spectrum Disorders. Rheumatology. 2015;54:1435-42.
- [CrossRef] [PubMed] [Google Scholar]
- Nailfold Capillaroscopy with USB Dermatoscope: A Cross-sectional Study in Healthy Adults. Indian J Dermatol Venereol Leprol. 2020;86:33-8.
- [CrossRef] [PubMed] [Google Scholar]
- Periungual Capillaroscopy in Psoriasis. An Bras Dermatol. 2012;87:550-3.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous and Systemic Psoriasis: Classifications and Classification for the Distinction. Front Med (Lausanne). 2021;8:649408.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and Management of the Metabolic Syndrome: An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735-52.
- [CrossRef] [PubMed] [Google Scholar]
- Nailfold Videocapillaro-Scopy Assessment of Microvascular Damage in Systemic Sclerosis. J Rheumatol. 2000;27:155-60.
- [Google Scholar]
- Nailfold Capillaroscopy in Rheumatic Diseases: Which Parameters Should be Evaluated? BioMed Res Int. 2015;2015:974530.
- [CrossRef] [PubMed] [Google Scholar]
- Nail-fold Capillaroscopy for the Dermatologists. Indian J Dermatol Venereol Leprol. 2022;88:300-12.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of Metabolic Syndrome in Patients with Psoriasis. Indian J Dermatol Venereol Leprol. 2010;76:662-5.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of Cardiovascular Risk Factors in Patients with Psoriasis. J Am Acad Dermatol. 2006;55:829-35.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of Metabolic Syndrome and Cardiovascular Changes in Patients with Chronic Plaque Psoriasis and Their Correlation with Disease Severity: A Hospital-based Cross-sectional Study. Indian J Dermatol Venereol Leprol. 2016;82:510-8.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of Metabolic Syndrome in Patients with Psoriasis: A Hospital-based Case-control Study. Br J Dermatol. 2007;157:68-73.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriasis, Metabolic Syndrome and Cardiovascular Risk Factors. A Population-based Study. J Euro Acad Dermatol Venereol. 2019;33:128-35.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriasis and Systemic Inflammatory Disorders. Int J Mol Sci. 2022;23:4457.
- [CrossRef] [PubMed] [Google Scholar]
- Risk of Psychiatric Diseases among Patients with Psoriasis in Korea: A 12-year Nationwide Population-based Cohort Study. J Dermatol. 2021;48:1763-71.
- [CrossRef] [PubMed] [Google Scholar]
- Risk of Non-alcoholic Fatty Liver Disease in Patients with Psoriasis: A Systematic Review and Meta-analysis. J Euro Acad Dermatol Venereol. 2015;29:656-62.
- [CrossRef] [PubMed] [Google Scholar]
- Risk of End-stage Renal Disease in Psoriatic Patients: Real-world Data from a Nationwide Population-based Cohort Study. Sci Rep. 2019;9:16581.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriasis and Metabolic Syndrome-scientific Evidence and Therapeutic Implications. J Med Life. 2014;7:468-71.
- [Google Scholar]
- Psoriasis and Metabolic Syndrome: Implications for the Management and Treatment of Psoriasis. J Euro Acad Dermatol Venereol. 2022;36:797-806.
- [CrossRef] [PubMed] [Google Scholar]







