Translate this page into:
Malignant Transformation of Linear Porokeratosis
*Corresponding author: Nidhin Niclavos, Department of Dermatology, St. John’s Medical College, Sarjapura Road, Bengaluru, Karnataka, India. nidhin.niclavos@stjohns.in
-
Received: ,
Accepted: ,
How to cite this article: Niclavos N, Aithal V. Malignant Transformation of Linear Porokeratosis. Indian J Postgrad Dermatol. 2025;3:56-8. doi: 10.25259/IJPGD_204_2024
Abstract
Porokeratosis (PK) is a rare disorder characterised by clonal expansion of keratinocytes without neoplastic transformation. However, malignant transformation, particularly to squamous cell carcinoma (SCC), is a documented complication. This case report describes a 58-year-old female with a 10-year history of progressively worsening, linear plaques on her left lower extremity. Skin biopsies initially suggested PK, leading to treatment with acitretin and cyclosporine. Subsequent biopsies revealed a moderately differentiating keratinising type of SCC arising within a background of linear PK. The patient ultimately underwent surgical excision and radiation therapy. This case highlights the potential for malignant transformation in PK, particularly the linear subtype. We review the literature on PK subtypes, risk factors for malignancy and management strategies. This case report emphasises the importance of clinical vigilance for malignant transformation in PK, particularly the linear variant. Early diagnosis and appropriate management are crucial for optimal patient outcomes.
Keywords
Linear porokeratosis
Malignant transformation
Porokeratosis
Squamous cell carcinoma
INTRODUCTION
Porokeratosis (PK) is a rare disorder characterised by non-neoplastic clonal expansion of keratinocytes. The classical form was described by Mibelli in 1893, subsequently, descriptions of superficial and disseminated forms of PK, linear porokeratosis (LP), disseminated superficial actinic porokeratosis (DSAP), disseminated palmoplantar PK and punctate PK were reported. Existing literature highlights the risk of progression to squamous cell carcinoma (SCC) in 6.4–16.4% of cases of PK.[1] Hence, it is imperative that clinical knowledge of this rare dermatosis is needed to differentiate it from clinically similar skin lesions for early diagnosis and screening.
CASE REPORT
A 58-year-old female presented with a 10-year history of progressively worsening, linear plaques on her left lower extremity. The eruption began as a single, tender papule on the foot that evolved into a verrucous, hyperplastic lesion. Over time, similar lesions developed proximally in a linear fashion, reaching the mid-thigh. These plaques were occasionally hypertrophic and discharged pus, especially with prolonged standing or exercise, but improved with antibiotics and steroids. Two prior skin biopsies were suggestive of PK, leading to treatment and mild resolution with oral acitretin and cyclosporine. On examination, linear hyperkeratotic plaques with irregular borders and a central furrow were present along the left lower limb, with some areas exhibiting verrucous changes and discharge [Figure 1]. Skin biopsies were performed again from multiple sites, followed by antibiotic therapy based on culture results. Based on the skin biopsy and soft-tissue ultrasound reports, a consultation with surgical oncology was obtained for further evaluation and management. The condition was finally managed with surgical excision and radiation therapy.
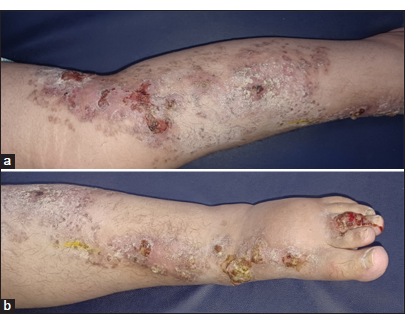
- (a) Linear hyperkeratotic plaques with irregular borders and a central furrow noted along the left lower limb. (b) Verrucous, hyperplastic plaques noted over the dorsum and third toe of the left foot.
Histopathology
Samples from the hyperplastic areas showed an ulceroinfiltrative malignant neoplasm arranged in nests and sheets with pseudoepitheliomatous hyperplasia. Atypical mitosis and keratin pearls were seen along with giant tumour cells. The dermis showed a dense lymphoplasmacytic infiltrate [Figure 2a]. The individual tumour cells were pleomorphic and squamoid, having a vesicular nucleus with prominent nucleoli and eosinophilic cytoplasm, intercellular bridges and individual cell keratinisation [Figure 2b]. The adjacent epidermis showed infundibular plugging with the cornoid process [Figure 2c]. The histopathological features are suggestive of moderately differentiating keratinising type of SCC in a background of LP.
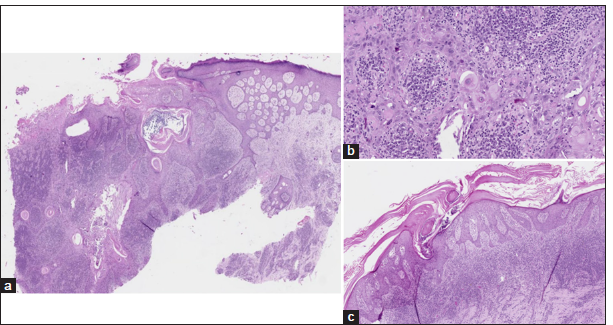
- (a) Pseudoepitheliomatous hyperplasia with the dermis shows a dense lymphoplasmacytic infiltrate (H&E 5x). (b) Pleomorphic and squamoid cells have vesicular nucleus with eosinophilic cytoplasm (H&E 20x). (c) Epidermis showing infundibular plugging with cornoid process (H&E 5x). H&E: Haematoxylin and eosin.
DISCUSSION
PK encompasses a spectrum of keratinisation disorders characterised by distinct clinical and histopathological features. These disorders typically manifest in early life as well-demarcated, hyperpigmented plaques with a characteristic raised, ridge-like border. Histologically, a cornoid lamella, a column of parakeratotic cells with pyknotic nuclei, is a defining feature observed at the periphery of the lesion. Several subtypes of PK exist, each with its clinical presentation and predilection for certain body sites. DSAP is the most common subtype, predominantly affecting sun-exposed areas in women during their third to fourth decade of life. Classic PK of Mibelli typically presents in young boys with a large lesion on an extremity and is associated with immunosuppression. Punctate PK and PK plantaris et palmaris disseminata are less frequent variants affecting the palms and soles, respectively. Although rare, the coexistence of multiple subtypes of PK in an individual has been documented in the literature.[2] A review of the literature shows that all forms of PK carry a potential, albeit low risk of malignant transformation. Notably, LP a rare unilateral subtype with lesions following Blaschko’s lines, carries a significantly higher risk (approximately 19%) compared to other PK types (7–11%).[2] The precise mechanism of malignant transformation remains elusive, but research suggests a role for the tumour suppressor gene p53. Mutations or functional inactivation of p53 can lead to uncontrolled cell proliferation and tumour development.[3] A review of the literature has shown that immunosuppression, ionising radiations and extensive lesions over a long duration can create a permissive environment for the uncontrolled growth of abnormal keratinocytes.[4] Management of SCC arising within PK lesions primarily involves wide surgical excision followed by close clinical follow-up for early detection of potential recurrences. While a standardised follow-up schedule is lacking, a personalised approach based on individual risk factors is recommended. These risk factors include the size and location of the primary lesion, the presence of lymph node involvement and the specific type of malignancy. The goal of follow-up is to detect locoregional recurrences, metastasis or development of new lesions as early as possible to initiate prompt treatment and improve patient outcomes.[5]
CONCLUSION
While most forms of PK exhibit a low risk of malignant transformation, LP carries a significantly higher risk. Understanding the risk factors associated with malignancy allows for development of personalised follow up strategies to detect potential malignancies as early as possible and ensure timely intervention.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship:
Nil.
References
- The Malignancy Potential of Porokeratosis: A Single Center Retrospective Study. Cureus. 2021;13:e13083.
- [CrossRef] [PubMed] [Google Scholar]
- Different Morphological Variants of Hypertrophic Porokeratosis and Disseminated Lesions of Porokeratosis of Mibelli: A Rare Co-existence. Indian J Dermatol Venereol Leprol. 2011;77:199-202.
- [CrossRef] [PubMed] [Google Scholar]
- p53, mdm-2, and p21 waf-1 in the Porokeratoses. Am J Dermatopathol. 1999;21:420-5.
- [CrossRef] [PubMed] [Google Scholar]
- p53 Alterations in Porokeratosis. J Cutan Pathol. 2003;30:455-8.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and Treatment of Invasive Squamous Cell Carcinoma of the Skin: European Consensus-based Interdisciplinary Guideline. Eur J Cancer. 2015;51:1989-2007.
- [CrossRef] [PubMed] [Google Scholar]








