Translate this page into:
Extramammary Paget’s Disease of Vulva: An Unusual Entity
*Corresponding author: Dhruv Rajiv Kabad, Department of Radiation Oncology, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India. drkabad@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kabad DR, Gupta S, Khan AA, Harishkumar P, Joseph D, Gupta M, et al. Extramammary Paget’s Disease of Vulva: An Unusual Entity. Indian J Postgrad Dermatol. doi: 10.25259/IJPGD_228_2024
Abstract
Extramammary Paget’s disease is a rare skin malignancy that presents as a primary lesion or can be an extension of an underlying adenocarcinoma. Primary extramammary Paget’s disease (EMPD) typically affects areas rich in apocrine sweat glands, such as perineum (vulva in this case). Localised form is surgically excised. However, extensive or metastatic form is treated with chemotherapy/radiotherapy or a combination of both. Data regarding treatment of extensive EMPD are limited.
Keywords
Extramammary Paget’s
Invasive
Liposomal doxorubicin
Vulva
INTRODUCTION
Paget disease (PD) comes in two varieties – Mammary PD (MPD) and extramammary PD (EMPD). MPD is a unique type of ductal carcinoma originating in the breast’s primary excretory ducts and spreading to the skin of the areola and nipple. EMPD is a rare skin malignancy of epithelial origin expressing apocrine or eccrine glandular-like features, characterised by Paget cells.[1] Paget cells have large pleomorphic centrally situated hyperchromatic nuclei, prominent nucleoli and abundant pale cytoplasm containing mucin.[2] Tumour cells are arranged singly or in nest-like groups primarily in the lower epidermis.[3] Delay in diagnosis results in dermal invasion of Paget cells resulting in invasive EMPD, which has a high tendency to metastasise.[4]
Wilkinson and Brown classified EMPD into primary and secondary. While the primary cutaneous EMPD originates from intra epidermal apocrine glands, secondary non-cutaneous EMPD can result from epidermotropic extension of an underlying internal adenocarcinoma.[5]
Primary EMPD typically affects areas rich in apocrine sweat glands, such as perineum, vulva, penis and scrotum. Vulva is the most common site of involvement, accounting for up to 60% of cases but fewer than 2% of original vulvar malignancies.[6]
Vulvar EMPD is more prevalent amongst Caucasians and menopausal women (mean age of presentation~70 years).[7]
Patients usually present with pruritus or burning pain and with an erythematous lesion with whitish ulcerations.
Currently surgical excision is the standard of treatment. If surgery is contraindicated, several alternative modalities include imiquimod 5% cream, photodynamic therapy (PDT), radiotherapy (RT) and chemotherapy.[8] In the present study, we discuss a case of EMPD of vulva with review of literature regarding its management strategies.
CASE REPORT
A 69-year postmenopausal lady presented with painful pruritic erythematous lesion in the perineum for 6 years. She was initially treated for fungal infection. There was symptomatic relief in pain and itching. Four years later, she visited a tertiary care hospital with complaints of severe pain and itching in the local lesion. Positron emission tomography scan done revealed fluorodeoxyglucose-avid diffuse cutaneous thickening with subcutaneous stranding in the vulva (standardised uptake value [SUV] max 9.3) with bilateral avid inguinal lymph nodes – largest left side (1.5 × 1.6 cm, SUV max 14.2). The patient underwent right inguinal lymph node biopsy [Figures 1 and 2] which was suggestive of metastatic adenocarcinoma Cytokeratin (CK)7+, CK20, Thyroid transcription factor 1 [TTF1-], GATA3+, Wilms tumour 1 [WT1-]). She was then referred to radiation oncology department of the same hospital where she received radical radiation.
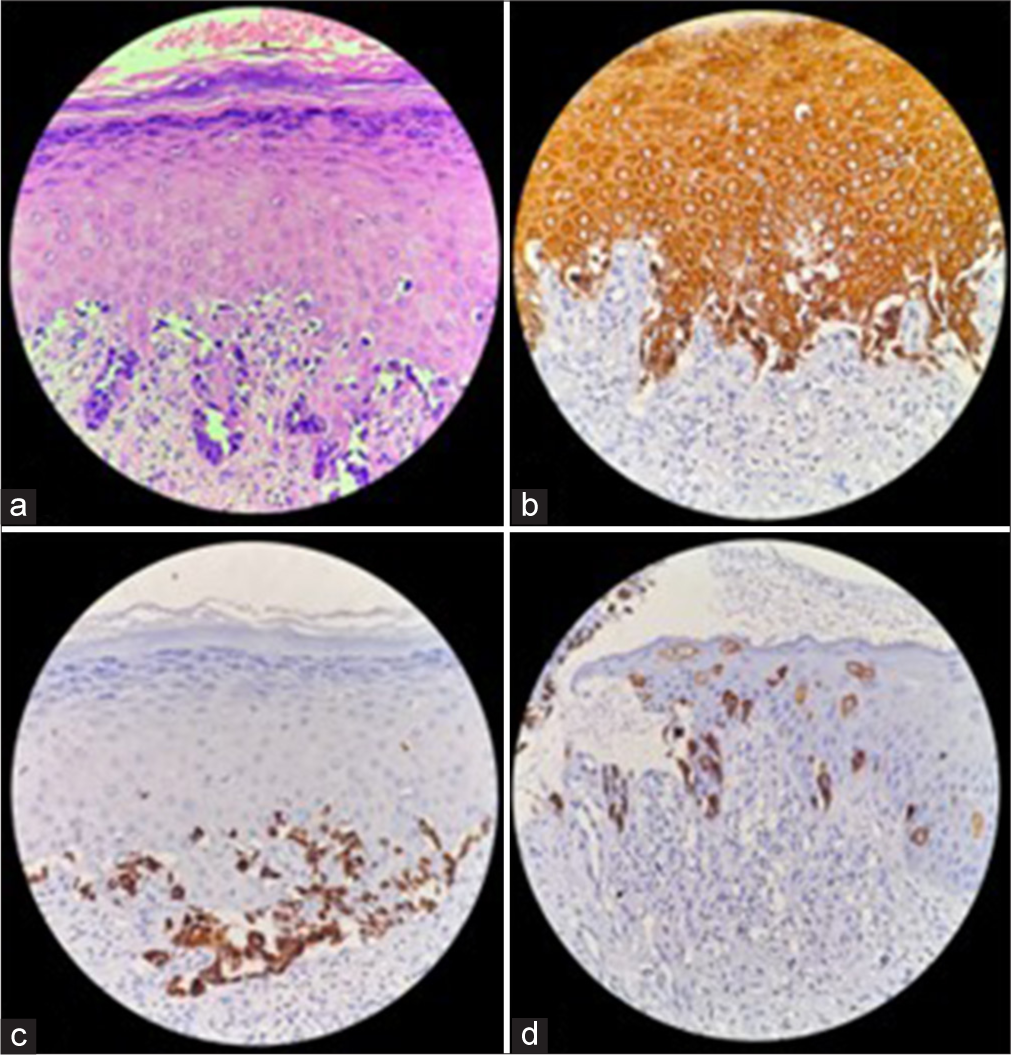
- (a) Haemotoxylin and eosin-stained section of the biopsy showing tissue lined by epidermis and a portion of superficial dermis. Note the characteristic large tumour cells (Paget cells) in singles and clusters just above the basal layer, having pale vacuolated cytoplasm. On IHC, these cells were positive for PanCK (b), CK7 (c) and EMA (d). (All images taken in ×400 view). PanCK: Pancytokeratin, EMA: Epithelial membrane antigen, CK: Cytokeratin, IHC: Immuno-histochemistry.
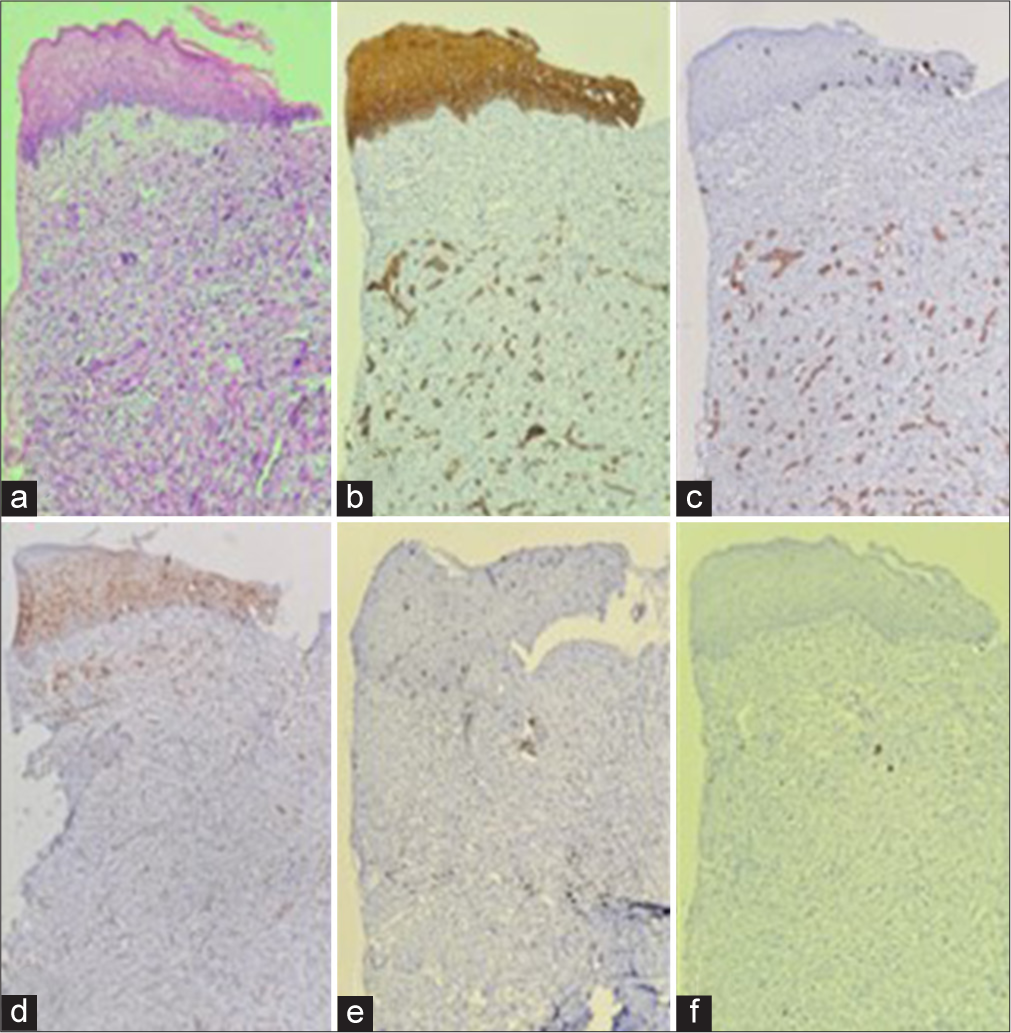
- (a) Focal area in the biopsy showing similar Paget cells in the epidermis along with invasion of these cells in the dermis. These cells are large, show nuclear pleomorphism, hyperchromatic irregular nuclei and vacuolated pale cytoplasm, Haemotoxylin and eosin stained. These cells were positive for PanCK (b), CK7 (c), EMA (d). GCDFP15 (e) showed focal non-specific staining in the tumour cells. These cells stained negative for CK20, HMB45, MelanA, P16 and P40 (All images taken in ×100 view). PanCK: Pancytokeratin, EMA: Epithelial membrane antigen, CK: Cytokeratin, HMB45: Human melanoma black, GCDFP: Gross cystic disease fluid protein.
The patient had a prolonged asymptomatic period of around 9-month postradiation after which she defaulted for further follow-up. She again developed pain at the vulvar lesion site and white discharge per vagina for which she visited gynaecology outpatient department at our institute with clinical description of lesion in Figure 3. In view of inoperable disease status, the patient was considered for palliative chemotherapy with liposomal doxorubicin (at 30 mg/m2 IV, 4 weekly cycles). The patient received 4 cycles of chemotherapy following which there was mild relief in symptoms, but clinically, the lesion was progressing. Multidisciplinary discussion was done, and in view of advanced age and progressive disease (PD), the patient was planned for best supportive care.

- Baseline image 10 × 8 cm ulceroproliferative growth involving bilateral labia majora/minora reaching up to inner aspect of bilateral thighs, 2 cm away from anal verge. Slough present.
DISCUSSION
We presented the case of primary invasive EMPD of vulva. EMPD is diagnosed primarily through biopsy. Immunohistochemistry is important to differentiate primary EMPD from secondary. Primary EMPD usually stains CK7(+), CK20(-), carcinoembryonic antigen (CEA)(+) and gross cystic disease fluid protein (GCDFP)-15(+), while secondary stains CK7(+), CK20(+) and GCDFP-15(−).[9] HER2 receptor mediated and androgen-receptor (AR) signalling have been implicated in the proliferation of Paget cells.[10]
It is usually diagnosed late due to its non-specific presentation in the form of pruritus, erythema and pain. Differential diagnoses include squamous cell carcinoma, leucoplakia, benign papulosquamous diseases and mycosis fungoides.[11] Therefore, early biopsy is recommended in patients with high suspicion.
Surgical excision has been accepted as the standard treatment for EMPD, which includes Mohs micrographic surgery, wide local excision, hemivulvectomy and complete vulvectomy with or without lymph node dissection depending on lesion size, depth of invasion, lymph node involvement or underlying adenocarcinomas. A margin of 2 cm is considered adequate during excision for primary EMPD.[12]
RT can be given in adjuvant setting or definite setting. In a study by Hata et al., 22 patients were identified with EMPD and received RT. Patients received a dose of 59.4–70.2 Gy (median 60.6 Gy) to the gross tumour (definitive intent) and those with positive surgical margins received a dose of 45– 64.8 Gy (median 50 Gy) to the tumour bed (adjuvant intent). The initial complete response rate was 100%. The study also concluded that for preventing lymph node metastasis, prophylactic RT to the regional lymph (pelvic and inguinal) nodes could be given to patients with invasive EMPD.[13]
Chemotherapy is the primary line of treatment for metastatic EMPD; however, its significance in its management is still under investigation. Due to the disease’s rarity and the dearth of scientific trials, opinions on the recommended course of chemotherapy for treatment are currently divided.
The role of 5-fluorouracil, epirubicin, carboplatin, vincristine and mitomycin C (FECOM) at 4 weekly intervals was evaluated by Oashi et al. which suggested partial response (PR) in 4 out of 7 eligible participants with EMPD, and the other 3 unevaluable patients also showed a decrease in the size of metastatic lesions. The most serious toxicities caused by FECOM were haematological.[14]
Yoshino et al., studied effects of single agent docetaxel in 13 patients with metastatic EMPD. Seven patients (58%) showed a PR, three (25%) stable disease and two (17%) PD. Patients treated with docetaxel experienced high rates of grade 3 or 4 myelosuppression.[15] Toxicity with docetaxel is myelosuppression and hypersensitivity.
Rationale behind using LipoDox in our index case was obtained from study conducted by Huang et al. wherein a 65-year postmenopausal lady with invasive EMPD and widespread metastases unresponsive to multiple lines of chemotherapy showed a remarkable response with LipoDox.[16] We were inclined towards using LipoDox due to favourable toxicity profile and convenient dosing regimen. Few toxicities associated with LipoDox are stomatitis, Hand–foot syndrome, Haematological and gastrointestinal symptoms. However, in our case, there was no response to LipoDox chemotherapy which could be attributed to possible drug resistance or aggressive tumour biology. Factors such as advanced age and patient defaulting for 6 years after initial treatment could be major contributors of poor response to therapy. Other setback was that we were unable to perform Immuno-histochemistry (IHC) test with androgen receptor and herceptin (Her2) receptor, which could have opened door for additional therapy.
CONCLUSION
EMPD is an uncommon female-dominated dermatological illness. Due to delayed diagnosis and high invasive disease rates, early detection is crucial. Standard of treatment is surgery; radiation can be used in definite or adjuvant forms. Various chemotherapeutic combinations have been used with varying outcomes.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Tumors of the Vulva In: , ed. WHO Classification of Tumours of Female Reproductive Organs (4th ed). Lyon, France: World Health Organization; 2014. p. :236-7.
- [Google Scholar]
- World Health Organization Classification of Tumours In: Pathology and Genetics Skin Tumours. Lyon: IARC; 2006. p. 13-9, 20-5, 137-8
- [Google Scholar]
- A proposal for a TNM Staging System for Extramammary Paget Disease: Retrospective Analysis of 301 Patients with Invasive Primary Tumors. J Dermatol Sci. 2016;83:234-9.
- [CrossRef] [PubMed] [Google Scholar]
- Vulvar Paget Disease of Urothelial Origin: A Report of Three Cases and a Proposed Classification of Vulvar Paget Disease. Hum Pathol. 2002;33:549-54.
- [CrossRef] [PubMed] [Google Scholar]
- Definition, Association with Malignancy, Biologic Behavior, and Treatment of Ectopic Extramammary Paget's Disease: A Review of the Literature. J Clin Aesthet Dermatol. 2019;12:40-4.
- [Google Scholar]
- Primary Extramammary Paget's Disease of the Vulva: The Clinicopathological Features and Treatment Outcomes in a Series of 43 Patients. Gynecol Oncol. 2013;129:412-6.
- [CrossRef] [PubMed] [Google Scholar]
- Three-Dimensional Evaluation Of Subclinical Extension Of Extramammary Paget Disease: Visualization of the Histological Border and Its Comparison to the Clinical Border. Br J Dermatol. 2017;177:229-37.
- [CrossRef] [PubMed] [Google Scholar]
- Metastatic Extramammary Paget's Disease: Pathogenesis and Novel Therapeutic Approach. Front Oncol. 2018;8:38.
- [CrossRef] [PubMed] [Google Scholar]
- Extramammary Paget's Disease: Analysis of Growth Signal Pathway from the Human Epidermal Growth Factor Receptor 2 Protein. Hum Pathol. 2005;36:1273-80.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term Outcome of Perianal Paget's Disease. Dis Colon Rectum. 2003;46:612-6.
- [CrossRef] [PubMed] [Google Scholar]
- Paget's Disease of the Vulva: Prevalence of Associated Vulvar Adenocarcinoma, Invasive Paget's Disease, and Recurrence after Surgical Excision. Am J Obstet Gynecol. 1999;180(1 Pt 1):24-7.
- [CrossRef] [PubMed] [Google Scholar]
- Role of Radiotherapy as Curative Treatment of Extramammary Paget's Disease. Int J Radiat Oncol Biol Phys. 2011;80:47-54.
- [CrossRef] [PubMed] [Google Scholar]
- Combination Chemotherapy for Metastatic Extramammary Paget Disease. Br J Dermatol. 2014;170:1354-7.
- [CrossRef] [PubMed] [Google Scholar]
- Usefulness of Docetaxel as First-line Chemotherapy for Metastatic Extramammary Paget's Disease. J Dermatol. 2016;43:633-7.
- [CrossRef] [PubMed] [Google Scholar]
- Liposomal Doxorubicin for Treatment of Metastatic Chemorefractory Vulvar Adenocarcinoma. Gynecol Oncol. 2002;87:313-8.
- [CrossRef] [PubMed] [Google Scholar]







