Translate this page into:
Cutaneous Leiomyomas
*Corresponding author: Iswariya Jaganathan, Department of Dermatology, Command Hospital (Airforce), Bengaluru, Karnataka, India. iswariyajaganathan@live.in
-
Received: ,
Accepted: ,
How to cite this article: Jaganathan I, Dinesh Kumar S, Bhatnagar A, Mitra D, Bahuguna A, Mutreja D. Cutaneous Leiomyomas. Indian J Postgrad Dermatol. doi: 10.25259/IJPGD_17_2024
Abstract
Leiomyoma is a benign tumour that frequently affects the genitourinary and gastrointestinal systems in adults. Cutaneous leiomyomas are rare benign tumours that originate from the hair follicle’s arrector pili muscle. Adults are more likely than children to develop cutaneous leiomyomas. There are three types: piloleiomyoma, dartoic leiomyoma and angioleiomyoma. We report ten cases of cutaneous leiomyoma with clinico-dermoscopic and histopathological evaluation, which, to the best of our knowledge, is being reported less frequently.
Keywords
Angioleiomyoma
Cutaneous
Dartoic
Dermoscopic
Histopathology
Leiomyoma
Piloleiomyoma
INTRODUCTION
Cutaneous leiomyomas are benign soft-tissue neoplasms that stem from the arrector pili muscle, the muscular layer of blood vessels, tunica dartos, labia majora, or nipple. The skin is the second most common location for leiomyoma after the uterus, contributing 5% of all leiomyomas. There are three types: Piloleiomyoma, dartoic leiomyoma and angioleiomyoma. They can occur sporadically or in association with uterine leiomyomas, or with renal abnormalities in Reed’s syndrome. Thorough evaluation and early diagnosis help to differentiate them from other skin and adnexal tumours, such as spindle cell tumours of fibrohistiocytic or peripheral nerve sheath origin. The definitive treatment is surgical excision. Other modalities include cryotherapy and ablative lasers along with pain management.
CASE SERIES
We report a case series of ten patients with cutaneous leiomyomas who were evaluated in terms of epidemiological, clinical, dermoscopic and histopathologic characteristics. Clinical demographic details and histopathological features were studied. In our case series, cutaneous leiomyomas were commonly observed among patients in their 3rd–5th decade, with a mean age at presentation of 45 years (30–56 years), female predominance and multiples in 70% of cases, with the maximum duration of the lesion noted being approximately 7 years. Sixty per cent of the patients complained of mild pain. On examination, multiple well-defined discrete nodules of varying size with an average diameter of 11.6 mm (10–15 mm) in about 70% of the cases are relatively soft to firm in consistency, non-mobile, smooth surface and skin over the lesion is normal.
The size of the nodule was <15 mm in five patients, between 10 and 15 mm in five patients, skin coloured in six cases and hyperpigmented in four cases. The most common sites encountered were the proximal and extensor aspects of the arms, followed by the upper chest and trunk [Figures 1 and 2]. Dermoscopy was done in all cases, which showed a well-defined, central homogenous yellowish area with polymorphous vessels in arborising and a linear pattern at the periphery. Pre-operative differential diagnoses were leiomyoma, dermatofibroma, neurofibroma, lipoma and pilomatricoma. Histologically, all lesions were compatible with cutaneous leiomyoma, with well-circumscribed spindle cell tumour arranged in fascicles with interlacing patterns. Immunohistochemical staining demonstrated diffuse positivity of actin-smooth muscle actin (SMA) in spindle cells, Ki 67 (<10%) and desmin [Figure 3]. All cases are summarised in Table 1.
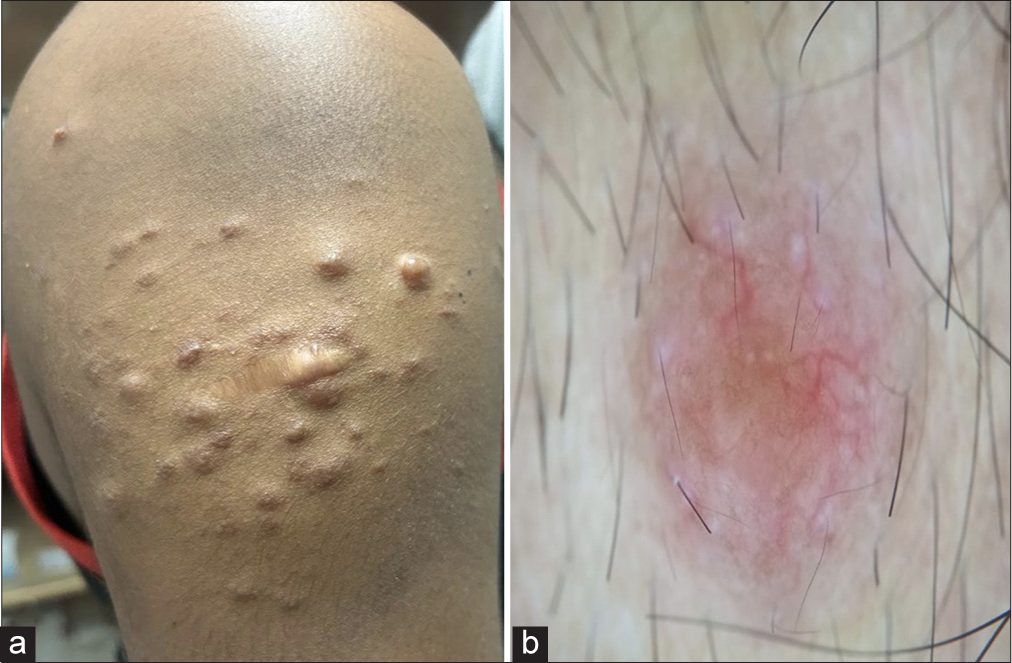
- (a) Multiple discrete skin coloured papules and nodules over the right arm. (b) Dermoscopy showing central homogenous yellowish areas with polymorphous vessels in arborising and linear pattern at the periphery (DermLite DL4-Contact/non-polarised mode).
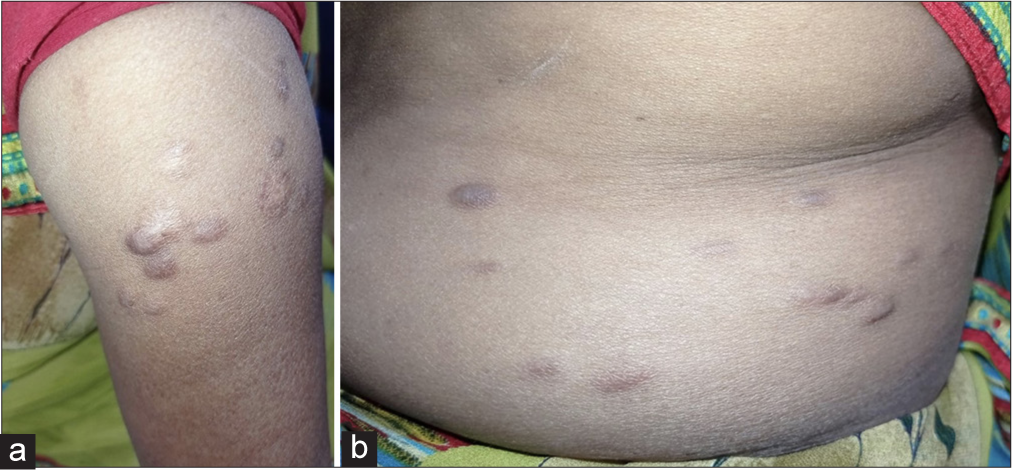
- (a) Multiple discrete to coalescing hyper and normopigmented papules and nodules over the right arm and (b) lateral aspect of trunk.
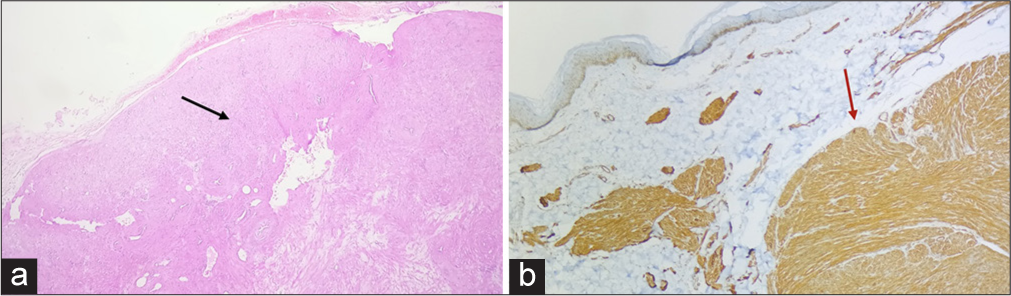
- (a) Histopathology: Spindle cell tumour arranged in fascicles with interlacing pattern (black arrow), elongated cells with eosinophilic cytoplasm and cigar shaped nuclei (10× magnification). (b) Immunohistochemistry: diffuse positivity (red arrow) of Smooth Muscle Actin.
| Case | Age (Years) | Sex | Duration (Years) | Number | Size max (mm) | Colour | Pain | Site | Clinical diagnosis |
|---|---|---|---|---|---|---|---|---|---|
| 1. | 51 | F | 7 | Multiple | 15×12 | Hyperpigmented | + | Trunk Forearms |
Leiomyoma Lipoma |
| 2. | 46 | F | 5 | Solitary | 15×10 | Skin coloured | − | Trunk | Dermatofibroma |
| 3. | 42 | F | 8 | Solitary | 12×10 | Hyperpigmented | − | Left elbow | Neurofibroma Lipoma |
| 4. | 41 | F | 6 | Multiple | 10×10 | Hyperpigmented | + | Arms Back |
Lipoma Leiomyoma |
| 5. | 56 | F | 5 | Multiple | 15×10 | Skin coloured | − | Trunk Neck |
Lipoma |
| 6. | 53 | F | 8 | Solitary | 12×10 | Skin coloured | Trunk | Dermatofibroma Angiolipoma |
|
| 7. | 46 | F | 6 | Multiple | 10×10 | Hyperpigmented | + | Arms | Leiomyoma Lipoma |
| 8. | 34 | M | 3.5 | Multiple | 15×10 | Skin coloured | + | Chest Arms |
Lipoma Leiomyoma |
| 9. | 36 | M | 3 | Multiple | 15×15 | Skin coloured | + | Arms Neck |
Lipoma Leiomyoma |
| 10. | 54 | M | 7 | Multiple | 12×10 | Skin coloured | + | Trunk Arms Shoulders |
Lipoma Leiomyoma Neurofibroma |
DISCUSSION
Cutaneous leiomyomas are uncommonly reported benign spindle cell tumours. The various types include (a) piloleiomyomas arising from the muscles of the arrector pili; (b) leiomyomas of genital sites originating from specialised smooth muscle of genital skin (dartoic, vulvar, mammillary, areolar) and (c) angioleiomyomas developing from smooth muscle tissue of the vessel wall.[1,2] Rare cases of pilar leiomyoma occur in infancy or in early childhood, the condition typically affects adults in their 3rd decade. The gender prevalence in our dataset may be attributed to women consulting more frequently due to aesthetic concerns.
Reed’s syndrome a rare genodermatosis with an autosomal dominant inheritance pattern caused by a mutation in the tumour suppressor gene fumarate hydratase.[3] The association of cutaneous leiomyomas with uterine leiomyomas and renal cell carcinoma is characteristic of hereditary leiomyomatosis and renal cell cancer syndrome.[4]
The common site predilection of arms and trunk observed in our case series is similar to previous reports, occurring in the 3rd and 5th decades. Female preponderance is predominantly multiple in number and of varying size. Dermoscopy showed well-defined, central homogenous yellowish areas with polymorphous vessels in an arborising and linear pattern at the periphery.
Histopathology reveals a dermal-based tumour with interlacing fascicles of spindle cells composed of abundant fibrillary eosinophilic cytoplasm and cigar-shaped nuclei. The surrounding collagen and subcutaneous fat are infiltrated by fascicles of aberrant spindle cells. Dermoscopic and histopathological correlation showed central homogenous yellowish structureless correlation to proliferation of spindle cells in dermis.[5]
Differential diagnoses include dermatofibroma, dermatofibrosarcoma, neurofibroma, lipoma, atypical fibroxanthoma, smooth muscle hamartomas, pleomorphic dermal sarcoma, schwannoma, malignant peripheral nerve sheath tumour, myopericytoma, adnexal tumours and cysts.
Surgical excision is the preferred mode of treatment with excellent prognosis and minimal recurrence. Long-term monitoring is necessary despite the minimal risk of malignancy. Additional data sets from larger case series could provide more insight into the histologic, clinical and prognostic features.
CONCLUSION
Cutaneous leiomyomas are benign tumours that originate from smooth muscle cells, typically appearing as firm, skin-colored or slightly pigmented nodules.
Dermoscopy plays a crucial role in the evaluation of cutaneous leiomyomas, revealing distinctive features that assist in diagnosis. Key dermoscopic features include a smooth and shiny surface, homogeneous skin-coloured or light brown areas with small, dotted / linear vascular structures and central hair follicle can occasionally be observed. Histopathologically, these tumours are characterised by haphazardly arranged bundles of smooth muscle fibers, often accompanied by a fibrous stroma. Understanding the dermoscopic, histopathological, and epidemiological features of cutaneous leiomyomas is essential for accurate diagnosis and management. While they are generally benign, awareness of their potential association with malignancies emphasizes the importance of thorough evaluation. Ultimately, recognizing these characteristics is vital for ensuring appropriate treatment and improving patient outcomes.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Pediatric Dermatopathology and Dermatology United States: Lippincott Williams and Wilkins; 2018.
- [Google Scholar]
- Superficial Leiomyomas. A Clinicopathologic Study of 34 Cases. Acta Pathol Jpn. 1987;37:1415-22.
- [CrossRef] [PubMed] [Google Scholar]
- Familial Cutaneous Leiomyomatosis. J Am Acad Dermatol. 1981;4:430-4.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic Features of Pilar Leiomyomas. Br J Dermatol. 2018;179:202-4.
- [CrossRef] [PubMed] [Google Scholar]








