Translate this page into:
CLOVES Syndrome: A Rare Disorder of Growth
*Corresponding author: Ayesha Sharmeen, Department of Dermatology, Jawaharlal Nehru Medical College, Aligarh Muslim University, Aligarh, Uttar Pradesh, India. sharmeenayesha2020@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Singhal A, Sharmeen A, Adil M, Amin SS. CLOVES Syndrome: A Rare Disorder of Growth. Indian J Postgrad Dermatol. 2024;2:121-5. doi: 10.25259/IJPGD_51_2024
Abstract
Congenital Lipomatous Overgrowth, Vascular malformations, Epidermal nevus and Skeletal abnormalities (CLOVES) syndrome is characterised by congenital lipomatous overgrowth, vascular malformations, epidermal nevi and skeletal anomalies without progressive or distorting bony overgrowth. A 10-month-old boy, born to nonconsanguineous and healthy parents, presented with congenital lipomatosis of the left side of face and verrucous epidermal nevus extending from the left pre- and post-auricular area, neck and upper left shoulder. He also had sandal gap deformity in both feet between 1st and 2nd toe. This case is being reported on account of its rarity, as till now, <150 cases has been reported worldwide.
Keywords
CLOVES syndrome
Epidermal nevus
Vascular malformations
Bony overgrowth
Proteus syndrome
INTRODUCTION
Congenital Lipomatous Overgrowth, Vascular malformations, Epidermal nevus and Skeletal abnormalities (CLOVES) syndrome, a relatively new overgrowth syndrome, is defined by the acronym CLOVES, which represents congenital lipomatous overgrowth, vascular anomalies, epidermal nevi and skeletal abnormalities.[1] The pathogenesis is associated with somatic (postzygotic) mutations in the PIK3CA gene located on chromosome 3q26.32.[2] CLOVES syndrome is exceptionally rare. The prevalence is fewer than one case per million individuals.[3]
CASE REPORT
A 10-month-old boy, born to otherwise non-consanguineous and healthy parents, presented to the outpatient department of dermatology with swelling over left side of face and pigmented skin lesions over neck since birth. The child had normal developmental milestones and was immunised for his age. His family and medical history showed no notable abnormalities. On examination, we noticed an asymmetrical swelling over left side of face extending from parietal bone up to the angle of mandible [Figure 1a] and verrucous epidermal nevus extending from left pre- and post-auricular area, neck and upper left shoulder [Figure 1b]. Sandal gap deformity was present bilaterally between 1st and 2nd toe, along with bilateral hypertrophy of the second toe of the feet [Figure 1c]. No bony, visceral, ocular and dental anomalies were detected. X-rays of both feet revealed widening of web spaces between 1st and 2nd toe and enlarged metapahalenges [Figure 2]. X-ray of whole abdomen revealed no abnormality [Figure 3]. Contrast-enhanced computed tomography head showed large non-capsulated subcutaneous fat extending from the left parietal bone to angle of mandible with fatty infiltration of the left parotid gland, masseter, temporalis, buccinator, lateral and medial pterygoid muscles, intrinsic and extrinsic muscles of left side of tongue muscle, hypertrophy of left mandible and left zygomatic arch [Figure 4]. Ultrasonography Doppler of the anterior abdominal wall mass showed no vascular malformation. Genetic workup was not done due to financial constraints and non-availability at our hospital.

- (a) Asymmetrical swelling over left side of face extending from parietal bone up to the angle of mandible, (b) verrucous epidermal nevus extending from left pre and post auricular area, neck and upper left shoulder and (c) sandal gap deformity between 1st and 2nd toe present bilaterally along with bilateral hypertrophy of the second toe of the feet.

- X-rays of both feet (anteroposterior and lateral view) showing widening of web spaces between 1st and 2nd toe and enlarged metapahalenges.

- X-ray of whole abdomen showing no abnormality.
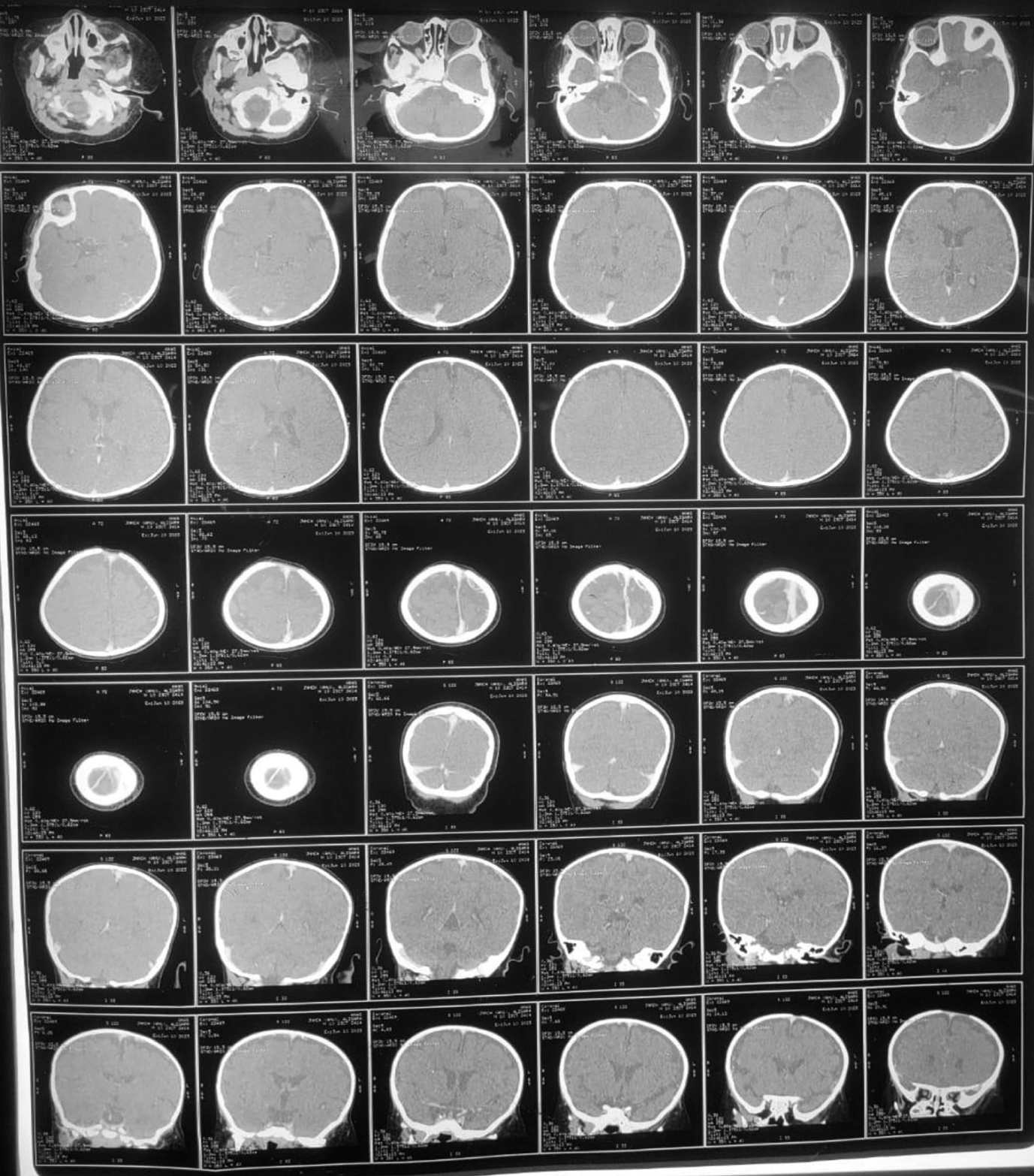
- Contrast-enhanced computed tomography head showing large non-capsulated subcutaneous fat extending from left parietal bone to angle of mandible with fatty infiltration of left parotid gland, masseter, temporalis, buccinator, lateral and medial pterygoid muscles, intrinsic and extrinsic muscles of the left side of tongue muscle, hypertrophied condylar process, hypertrophy of left mandible and left zygomatic arch.
DISCUSSION
CLOVES syndrome (OMIM number 612918) is a rare, sporadic and complex mosaic overgrowth syndrome. It is now classified under the umbrella of PIK3CA-Related Overgrowth Spectrum (PROS) characterised by postzygotic activating somatic mutations in the PIK3CA gene, which is located on chromosome 3q26.32.[4] It presents as congenital overgrowth of adipose tissue across various body regions and tissue spaces and unilateral or bilateral lipomatous masses, particularly prominent on the thoracic and abdominal walls.[5] CLOVES syndrome is characterised by capillary malformation (including low-flow and geographic patterns), venous anomalies (such as superficial phlebectasia), lymphatic abnormalities (including macrocystic, microcystic or mixed presentations) and arteriovenous malformations.[5] Epidermal nevi is either congenital or develop in childhood and is usually found on the neck, abdomen, flank or limbs. Skeletal malformations in CLOVES syndrome often present as scoliosis and asymmetric enlargement of skeletal structures in the extremities. Scoliosis may be congenital or develop during childhood, possibly due to lower limb asymmetry.[6] Other musculoskeletal manifestations include leg length discrepancy, genu recurvatum, polydactyly, syndactyly, splayed feet and sandal gap (widened first toe web).[7]
The diagnosis of CLOVES syndrome remains clinical, but it must be differentiated from other PROS disorders, particularly from Proteus syndrome and Klippel-Trenaunay syndrome, as mentioned in Table 1.[8,9]
| Features | CLOVES syndrome | Proteus syndrome | Klippel-Trenaunay syndrome |
|---|---|---|---|
| Mutations | PIK3CA gene | AKT-1 gene | PIK3CA gene |
| Presentation | Overgrowth features present at birth, asymmetric, disproportionate and less progressive | Overgrowth features seen at 6–18 months of life, become severe with advancing age | Capillary hemangioma or port-wine stain presents at birth, during early infancy, or childhood. Limb hypertrophy may be observed at birth, typically progressing further during the first years of life |
| Cutaneous | Phlebectasia, epidermal nevi | Soft-tissue overgrowth, cerebriform overgrowth over palms and soles | Vascular malformation, port-wine stain |
| Fat malformations | Congenital fat hamartoma can affect the trunk, face, limbs and scrotum, and may extend into the retroperitoneum, epidural space, thoracic cavity, or mediastinum | Acquired fat hypertrophy | Acquired extrafascial/subcutaneous fat overgrowth |
| Vascular malformations | Phlebectasia, low-flow and high-flow vascular anomalies, CM, VM, LM and spinal AVM | CM, VM and LM | CM (port-wine stain), VM (marginal venous system), LM affecting lower limb in most cases and no high-flow component |
| Skeletal anomalies | Asymmetric lower limb, scoliosis and pectum excavatum | Scoliosis, lower limb asymmetry, soft and bone tissue hypertrophy | Soft and bone tissue hypertrophy, lower limb asymmetry |
| Acral anamolies | Macrodactyly, polydactyly, syndactyly and sandal gap. Present at birth and slowly increase with growth | Asymmetric and disproportionate acral overgrowth, Macrodactyly | Macrodactyly, polydactyly and syndactyly |
| Neural anamolies | Hemi-megalencephaly, seizures and corpus callosum dysgenesis | Hemi-megalencephaly, developmental delay | Hemi-megalencephaly, seizures, developmental delay and spina bifida |
| Complications | Scoliosis, haemoptysis, cardiac failure from AVM, pulmonary embolism, gastrointestinal bleeding/obstruction | Hyperostosis, developmental delay, benign and malignant tumours, restrictive lung functions, pulmonary embolism, DVT | Developmental delay, DIC, pulmonary thromboembolism, Kassabach–Merrit syndrome and superficial thrombophlebitis |
CM: Capillary malformation, VM: Venous malformation, LM: Lymphatic malformation, AVM: Arteriovenous malformation, DIC: Disseminated intravascular coagulopathy, DVT: Deep venous thrombosis. Modified after Martinez-Lopez A, et al.[9] CLOVES: Congenital Lipomatous Overgrowth, Vascular malformations, Epidermal nevus and Skeletal abnormalities. The clinical feature of CLOVES syndrome noted here in bold were present in the index case.
We made the diagnosis of CLOVES syndrome in our patient based on diagnostic criteria by Keppler-Noreuil et al., as mentioned in Table 2.[8,9]
| Criteria | Features | Remarks |
|---|---|---|
| Required | Presence of somatic PIK3CA mutation Congenital or early childhood onset Overgrowth sporadic and mosaic |
If no mutation identified, then consider a presumptive diagnosis of PROS - - |
| Spectrum (require two or more features) | Overgrowth: Adipose, muscle, nerve and skeletal Vascular malformations: capillary, venous, lymphatic, arteriovenous malformations Epidermal nevus Hemi-megalencephaly |
Typically progressive. Can manifest as scoliosis, limb overgrowth, CNS anomalies (hydrocephalus, cerebellar tonsillar ectopia, Chiari, megalencephaly, mega corpus callosum), regional lipomatous undergrowth with overgrowth, infiltrating lipomatosis, Wilms tumour/ovarian cystadenoma |
| Isolated features | Large isolated lymphatic malformation Isolated macrodactyly or overgrown splayed feet/hands, overgrown limbs Truncal adipose overgrowth Dysplastic megalencephaly/focal cortical Epidermal nevus Seborrheic keratoses Benign lichenoides keratoses |
- - - - - - - |
PROS: PIK3CA-related overgrowth spectrum, CNS: Central nervous system
Managing CLOVES syndrome requires a comprehensive, multidisciplinary approach personalised to each patient’s specific needs. Treatment strategies include surgical debulking for lipomatous overgrowths, sclerotherapy and embolisation for vascular malformations, pulse-dye lasers for capillary malformations and epiphysiodesis for limb length discrepancies.[10] The Food and Drug Administration granted accelerated approval to Alpelisib (Vijoice, Novartis Pharmaceuticals) on 5 April 2022, for treating severe manifestations of PROS in adult and paediatric patients aged 2 years and older who need systemic therapy.[11]
CONCLUSION
CLOVES syndrome is exceptionally rare, and research in this area is predominantly limited to a scant body of published literature. Herein, we report a case of a 10-month-old baby with CLOVES syndrome. We are presenting this case to contribute to medical literature by providing a comprehensive account on CLOVES syndrome.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Newly Delineated Syndrome of Congenital Lipomatous Overgrowth, Vascular Malformations, and Epidermal Nevi (CLOVE Syndrome) in Seven Patients. Am J Med Genet. 2007;143A:2944-58.
- [CrossRef] [PubMed] [Google Scholar]
- Somatic Mosaic Activating Mutations in PIK3CA Cause CLOVES Syndrome. Am J Hum Genet. 2012;90:1108-15.
- [CrossRef] [PubMed] [Google Scholar]
- An Extremely Rare Disorder of Somatic Mosaicism. Adv Neonat Care. 2016;16:347-59.
- [CrossRef] [PubMed] [Google Scholar]
- A Review on Cutaneous and Musculoskeletal Manifestations of CLOVES Syndrome. Clin Cosmet Investig Dermatol. 2022;15:621-30.
- [CrossRef] [PubMed] [Google Scholar]
- CLOVES Syndrome: Severe Neonatal Presentation. J Clin Diagn Res. 2017;11:TR01-3.
- [CrossRef] [PubMed] [Google Scholar]
- Cloves Syndrome: A Rare Disorder of Overgrowth with Unusual Features-An Uncommon Phenotype? Indian Dermatol Online J. 2019;10:447-52.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical Profile of Overgrowth Syndromes Consistent with PROS (PIK3CA-Related Overgrowth Syndromes)-A Case Series. Indian Dermatol Online J. 2020;11:738-46.
- [CrossRef] [PubMed] [Google Scholar]
- PIK3CA-related Overgrowth Spectrum (PROS): Diagnostic and Testing Eligibility Criteria, Differential Diagnosis, and Evaluation. Am J Med Genet A. 2015;167A:287-95.
- [CrossRef] [PubMed] [Google Scholar]
- CLOVES Syndrome: Review of a PIK3CA-related Overgrowth Spectrum (PROS) Clin Genet. 2017;91:14-21.
- [CrossRef] [PubMed] [Google Scholar]
- Sonographic Screening for Wilms Tumor in Children with CLOVES Syndrome. Pediatr Blood Cancer. 2017;64:e26684.
- [CrossRef] [PubMed] [Google Scholar]
- Alpelisib: A Novel Agent for PIK3CA-Related Overgrowth Spectrum. J Pediatr Pharmacol Ther. 2023;28:590-4.
- [CrossRef] [PubMed] [Google Scholar]







