Translate this page into:
An Asymptomatic Nodular Lesion Over the Forearm – A Diagnostic Dilemma
*Corresponding author: Shravya Shetty, Department of Dermatology, Kanachur Institute of Medical Sciences, Mangaluru, Karnataka, India. shravyashetty23@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shetty S, Shenoi SD, Meghashree G, Kumar K, Shetty SA. An Asymptomatic Nodular Lesion Over the Forearm – A Diagnostic Dilemma. Indian J Postgrad Dermatol. 2025;3:59-61. doi: 10.25259/IJPGD_88_2024
CASE DESCRIPTION
A 27-year-old woman presented to the dermatology outpatient department with a painless, hard swelling over her left forearm for 3 years. Clinical examination revealed a 3 × 3 cm firm to hard, lobulated nodule over the extensor aspect of the left forearm [Figure 1a]. The overlying skin was atrophic with pigmentary changes and discolouration. Dermoscopic examination revealed a whitish structureless area with irregular linear vessels [Figure 1b]. Surgical excision was planned, and ultrasonography of soft tissue was performed, which showed a well-defined lesion with peripheral calcification in the subcutaneous tissue of the dorsal aspect of the mid-forearm with no vascularity or surrounding changes, indicating a calcified epidermoid cyst [Figure 1c]. After the nodule was excised, it was sent for histopathological examination.
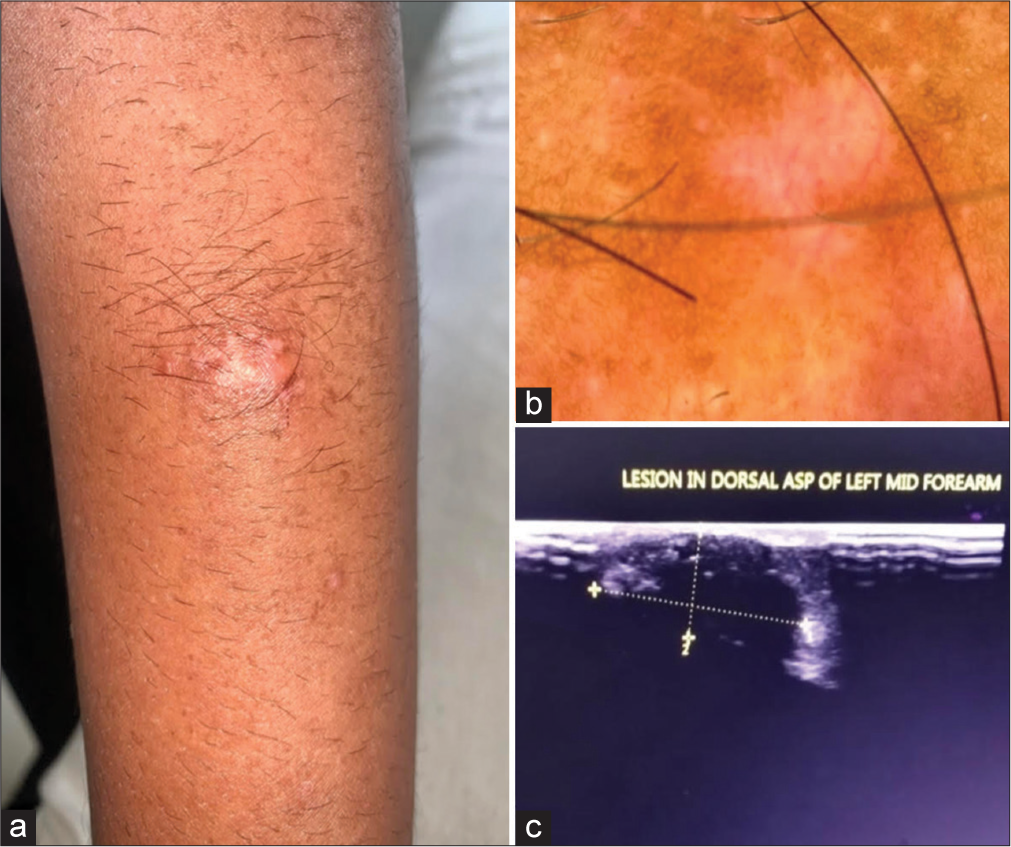
- (a) Firm to hard lobulated nodule over the left forearm measuring 3 × 3 cm with pigmentary changes. (b) Dermatoscopic examination revealing a whitish structureless area with an erythematous hue. (c) Ultrasonography of soft tissue shows a well-defined lesion with peripheral calcification in the subcutaneous tissue with no vascularity or surrounding changes, indicating a calcified cyst.
HISTOPATHOLOGIC FINDINGS
Histopathological examination revealed an adnexal neoplasm that was well-circumscribed, lobulated, and composed of several islands of basaloid cells, some of which exhibited abrupt keratinisation. Plenty of ghost cells with surrounding stroma showed calcification suggestive of pilomatricoma [Figure 2].
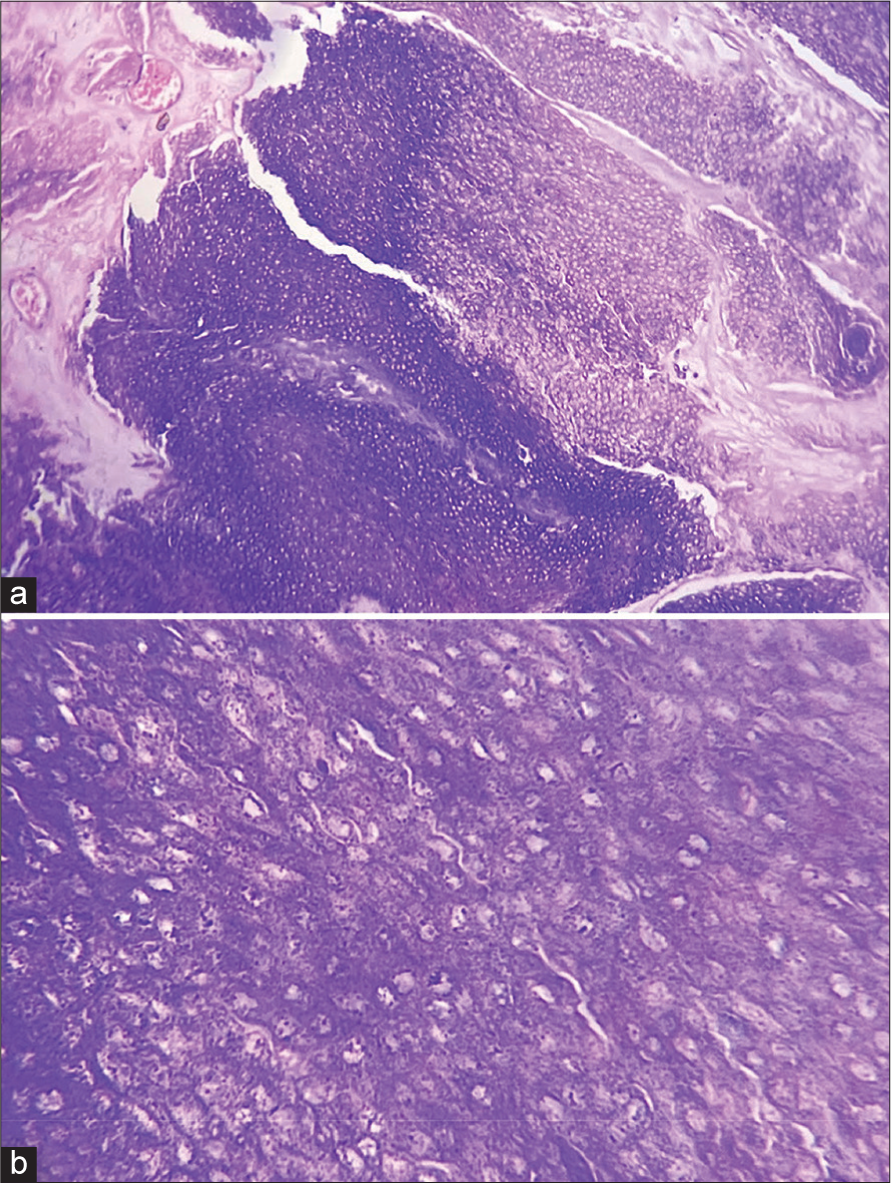
- (a) A well-demarcated tumour containing calcifications, foreign body cells, and ghost cells with eosinophilic cytoplasm and islands of epithelial cells, including basaloid matrical cells (H&E, ×10), (b) anucleated ghost (or shadow) cells (H&E, ×40). H&E: Haematoxylin and eosin.
DIAGNOSIS
Pilomatricoma.
DISCUSSION
Pilomatricoma, also called as Calcifying Epithelioma of Malherbe, is a benign slow-growing neoplasm of the skin arising from the hair follicles, which frequently appears as an asymptomatic solitary, firm nodule, displaying a normal to pearl white epidermis. These tumour cells can develop into the outer root sheath, hair bulge, follicular infundibulum, hair cortex, and hair matrix. Ninety percentage of cases involve individuals younger than 10 years old. While it primarily affects the head and neck regions that bear hair, it can also affect the trunk and extremities. Stretching the skin may reveal the tent sign, a flattened portion of the lesion with an angle resembling a tent.[1]
Studies indicate that pilomatricoma may be related to a mutation in exon 3 of the B-catenin gene, yet the exact cause of the condition is still unknown.[2] As a component of the cadherin protein, B-catenin plays a crucial role in the differentiation of hair follicles. It shows positivity for BCL23 and LEF-1 (a marker for hair matrix cells). Multiple or familial pilomatricomas have been notably associated with several conditions, including Gardner syndrome, xeroderma pigmentosum, myotonic dystrophy, and basal cell nevus syndrome.[3] Histopathology of pilomatricoma reveals a tumour that is well-demarcated and encapsulated. Cells from the dermis infiltrate into the subcutaneous tissue. The tissue contains calcifications, foreign body cells, ghost cells (shadow or anucleated cells) with eosinophilic cytoplasm, and islands of epithelial cells, including basaloid metrical cells.
Ultrasound can be used to illustrate posterior shadowing, calcifications, heterogeneous echotexture, and hypoechoic rim.
When indicated, surgical excision is the preferred treatment. The likelihood of recurrence is low, estimated at 2–6%, possibly attributed to incomplete excision.
Calcinosis cutis, epidermoid cysts, neurofibromas, chondromas, fibroxanthomas, hematomas, osteoma cutis, and giant cell tumours are among the various differential diagnoses to consider.
Although uncommon with fewer than 20 cases reported, rarely it can undergo malignant transformation.[4] Higher cellular pleomorphism, an accelerated rate of mitosis, atypia, central necrosis, as well as higher infiltration into the surrounding soft tissue, lymphatic arteries, skin, and blood are all common characteristics of pilomatricomas that have an enhanced tendency for malignant transformation. In men between the fifth and seventh decades of life, these frequently manifest as firm, non-tender nodules on the head or neck. About 10% of instances have the tumour spread to other organs, most often the lungs, and local recurrence is a predictor of this. Excision with wide margins is the treatment of choice; however, it carries a high rate of recurrence rate ranging from 50 to 60%. For recurrent or metastatic disease, adjuvant radiation therapy or chemotherapy is employed.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Beta-catenin Mutation and Its Nuclear Localization are Confirmed to be Frequent Causes of Wnt Signaling Pathway Activation in Pilomatricomas. J Dermatol Sci. 2006;41:67-75.
- [CrossRef] [Google Scholar]
- Calcifying Epithelioma of Malherbe. Association with Myotonic Muscular Dystrophy. Arch Dermatol. 1972;106:41-4.
- [CrossRef] [Google Scholar]
- Malignant Pilomatricoma in the Parietal Area. Pathol Oncol Res. 2006;12:251-3.
- [CrossRef] [Google Scholar]






