Translate this page into:
Palmoplantar Painful Pitted Keratotic Papules: A Unique Presentation of Discoid Lupus Erythematosus Coexisting with Systemic Lupus Erythematosus
*Corresponding author: Anil Budania, Department of Dermatology, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India. anilbuddy25@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kumar S, Bano N, Kaur M, Budania A, Nalwa A. Palmoplantar Painful Pitted Keratotic Papules: A Unique Presentation of Discoid Lupus Erythematosus Coexisting with Systemic Lupus Erythematosus. Indian J Postgrad Dermatol. doi: 10.25259/IJPGD_178_2024
Dear Editor,
Discoid lupus erythematosus (DLE) is the most common subset of chronic cutaneous lupus erythematosus.[1] DLE typically affects the head and neck with scarring alopecia. Palmoplantar DLE is rare, often presenting as painful erythematous plaques or erosions.[2] We report a rare case of palmoplantar DLE presenting with keratotic pitted painful papules, a unique manifestation that warrants attention due to its diagnostic and therapeutic complexities.
A 65-year-old male presented with complaints of multiple painful erythematous palmoplantar lesions hampering his daily activities for 2 years. He denied any associated history suggestive of connective tissue diseases, including photosensitivity, Raynaud’s phenomenon, skin tightness, arthritis, respiratory difficulty, proximal muscle weakness, etc. Examination revealed bilateral symmetrical involved of palms and soles having multiple discrete to grouped haemorrhagic vesicles with overlying crusting and erythematous to atrophic scaly plaques with multiple palmoplantar pits and keratotic pitted papules predominantly localised to ventral and lateral aspect of foot. Prominent erythema was noted at margins of plaques [Figure 1]. Systemic examination was unremarkable.
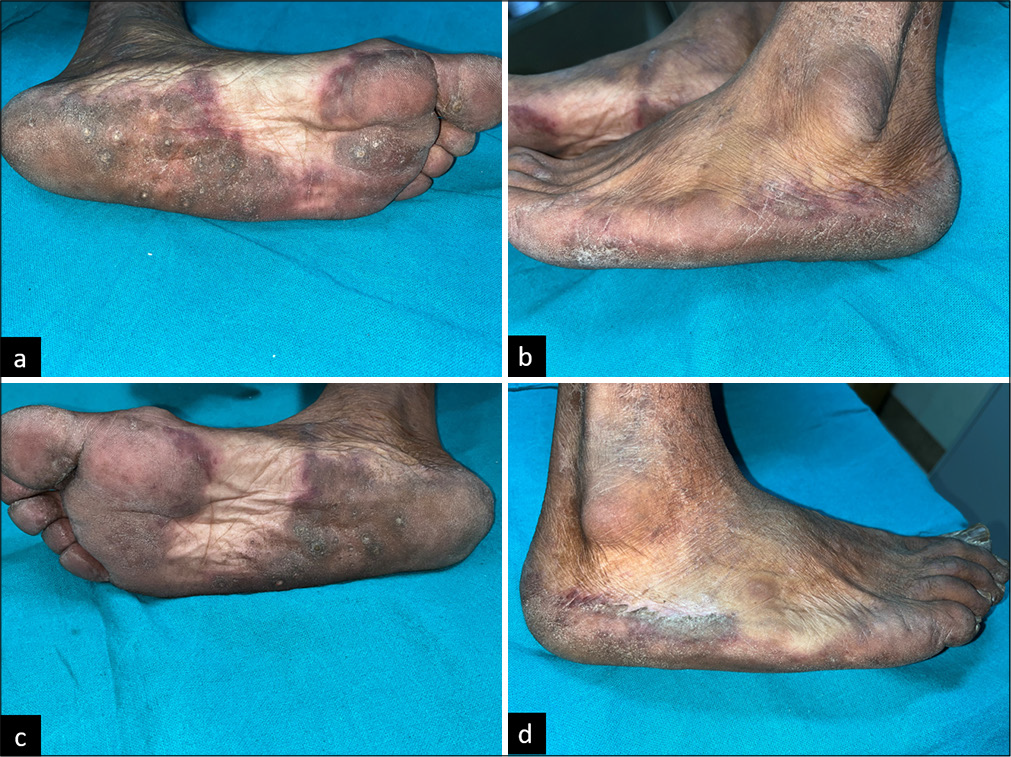
- Left foot plantar aspect showing well-defined erythematous plaque with (a) multiple keratotic pitted papules, lateral border of left foot showing (b) prominent erythema, right foot plantar aspect showing well defined erythematous plaque with (c) multiple keratotic pitted papules and lateral border of right foot showing (d) prominent erythema.
One year later, the patient developed erythematous lesions over neck, chest, extensors of upper limb with associated burning, itching and photosensitivity while palmoplantar lesions persists almost as it is with mild fluctuation in severity for a year. Examination revealed malar rash, erythematous maculopapular rash with crusting over neck, chest and upper limb and bullous lesions with surrounding painful erythema over palm and soles [Figure 2]. Systemic examination was unremarkable. Baseline routine investigations including complete hemogram, kidney function test, liver function test, urine routine microscopy, urine 24-h protein and chest X-ray came within normal limit. Antinuclear antibody (ANA) (by indirect immunofluorescence) came positive with titre of 3+, nuclear and speckled pattern. A 4 mm punch biopsy was taken from erythematous plaque over left foot which revealed focal basal cell vacuolisation and occasional apoptotic keratinocytes with moderate superficial and deep dermal periadenexal and perivascular oedema with mild lymphocytic infiltrate. No evidence of dermal mucin is noted. Direct immunofluorescence (DIF) was negative for immunoglobulin (Ig)A, IgG and C3 [Figure 3]. Repeat ANA profile showed anti-Smith antibody borderline positive and anti-Sjogren-syndrome related antigen A and antigen B (SSA and SSB) antibody strong positive. Systemic evaluation was within normal limits.

- Erythematous maculopapular rash with crusting over neck and chest.
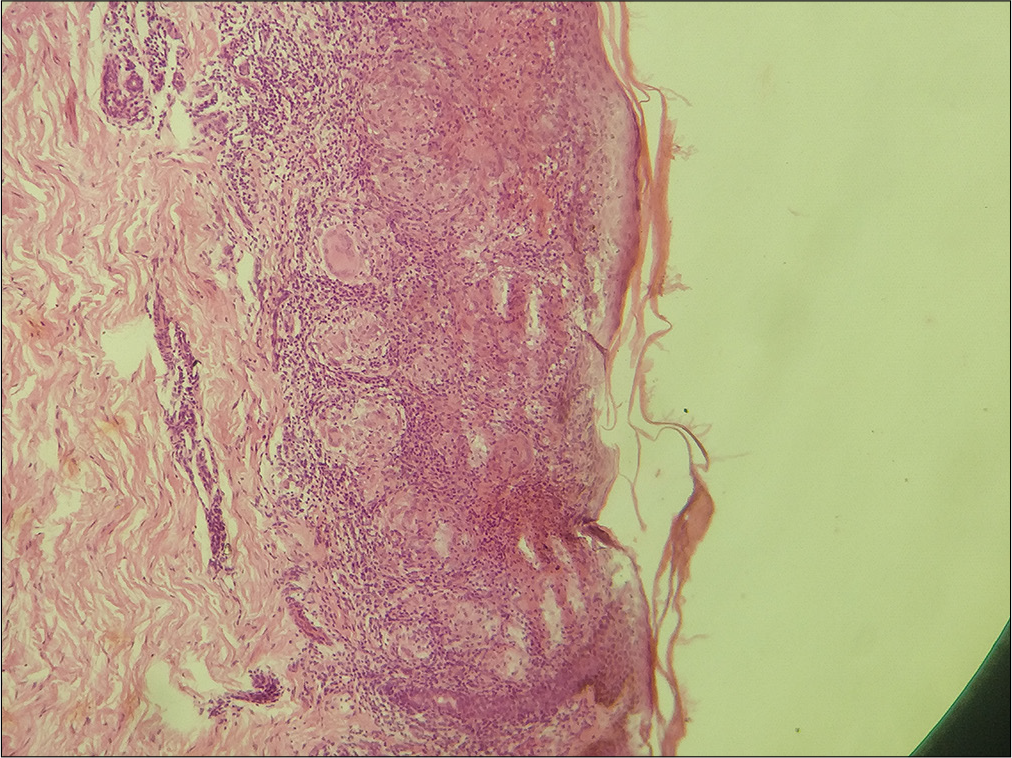
- Histopathology image (Haematoxylin and eosin stain, ×40 magnification) shows focal basal cell vacuolisation and occasional apoptotic keratinocytes with moderate superficial and deep dermal periadenexal and perivascular oedema with mild lymphocytic infiltrate.
Taking into consideration keratotic palmoplantar pits with erythematous plaques, differential diagnosis of palmoplantar lichen planus, palmoplantar DLE, lichen planus-lupus erythematosus overlap syndrome and acquired palmoplantar keratoderma (PPK) were kept. Acquired PPK was ruled out based on presence of other symptoms such as malar rash, erythematous maculopapular rash over photo-exposed sites, strong positive ANA and histopathological findings. Lichen planus was ruled out based on histopathological findings including superficial and deep dermal, perivascular and periadenexal lymphocytic infiltrate and absence of band like infiltrate at dermo-epidermal junction which favours DLE.
Final diagnosis of palmoplantar DLE progressed to systemic lupus erythematosus was made considering strong positive ANA and characteristic histopathology findings consistent with DLE even in absence of mucin and negative DIF.
Initially, the patient was started on tablet hydroxychloroquine 300 mg once per day, tablet prednisolone 40 mg once per day and tablet methotrexate 15 mg once per week. He showed moderate improvement for initial 1–2 months, but recurrence occurred after 3 months, while on same treatment and treatment was changed from methotrexate to azathioprine 50 mg twice per day.
After second recurrence with new-onset malar rash and erythematous crusted maculopapular rash over photo-exposed sites, he was managed with tablet prednisolone 60 mg once per day with continuation of azathioprine 50 mg once per day and hydroxychloroquine 300 mg once per day and is currently under follow-up with good improvement.
DLE is considered as the most common variant of chronic cutaneous lupus erythematosus. Palmoplantar DLE is challenging to diagnose and manage due to its rarity and diverse clinical presentations. This unique case demonstrates the importance of considering atypical clinical features, such as keratotic pitted papules, in the differential diagnosis of palmoplantar lesions of DLE. Approximately 1/4th of systemic lupus erythematosus (SLE) patients developed DLE lesions at some point during their disease course. In this case report, the patient presented with palmoplantar DLE which later progressed to SLE within 1 year. DLE of the palms and soles may manifest classically as discoid lesions as well as erythematous scaly plaques: the painfully erosive variant is observed in <2% of patients and is often a diagnostic challenge. DLE involving palm and soles is debilitating disease due to severe pain, refractory to treatment and additionally increase risk of squamous cell carcinoma development due to chronic course.[3] Various rare presentation of DLE such as prurigo nodularis such as lesions, bullous, annular, telangiectode, linear along Blaschko’s lines and atrophie blanchelike lesions have been reported in the literature.[1] This case is further adding one rarer variant of palmoplantar DLE having painful keratotic pitted papules and plaques. In addition, absence of mucin and DIF negativity in this case further makes it more interesting and difficult to diagnose. However, absence of mucin in DLE has already been reported by Cawley et al.[4] and DIF negativity in approximately 32% cases of DLE by Bharti et al.[5] Palmoplantar lesions of DLE are usually resistant to conventional treatment of DLE including potent topical steroids, intralesional steroids, hydroxychloroquine, dapsone and systemic immunosuppressive therapy. Mycophenolate mofetil has also been tried with successful treatment of palmoplantar lesions of recalcitrant DLE. [2] This case report enlightens various unique features such as presence of pitted painful keratotic papules and plaques over palm and sole which are recalcitrant to treatment, chronic relapsing remitting course, initial presentation as palmoplantar DLE which later progression to SLE and absence of mucin with negative DIF on lesional histopathological examination.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Hair and Scalp Changes in Cutaneous and Systemic Lupus Erythematosus. Am J Clin Dermatol. 2018;19:679-94.
- [CrossRef] [PubMed] [Google Scholar]
- Overview of Common, Rare and Atypical Manifestations of Cutaneous Lupus Erythematosus and Histopathological Correlates. Lupus. 2010;19:1050-70.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of Resistant Discoid Lupus Erythematosus of the Palms and Soles with Mycophenolate Mofetil. J Am Acad Dermatol. 2001;45:142-4.
- [CrossRef] [PubMed] [Google Scholar]
- An Examination of Skin from Patients with Collagen Disease Utilizing the Combined Alcian Blue-periodic Acid Schiff Stain. J Invest Dermatol. 1956;27:389-94.
- [CrossRef] [PubMed] [Google Scholar]
- Immunofluorescence Profile of Discoid Lupus Erythematosus. Indian J Pathol Microbiol. 2015;58:479-82.
- [CrossRef] [PubMed] [Google Scholar]







