Translate this page into:
Oral Mucosal Swelling: Not all Lesions are Doomed
*Corresponding author: Savi Aneja, Department of Dermatology, Government Medical College and Hospital, Chandigarh, India. anejasavi@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Aneja S, Arora A, Thami GP, Jain T. Oral Mucosal Swelling: Not all Lesions are Doomed. Indian J Postgrad Dermatol. 2025;3:97-8. doi: 10.25259/IJPGD_221_2024
Dear Editor,
Oral mucosal swellings are seen in day-to-day clinical practise. Majority of the oral mucosal swellings are benign, causes include mucocele, dermoid and epidermoid cysts, ranula and benign tumours of salivary gland. Another important benign cause of oral swelling is intraoral lipoma. Lipomas are the most common soft-tissue neoplasms affecting approximately 1% of people. Approximately 15–20% of cases occur in the head-and-neck region, while only 1–4% are found in the oral cavity, making it a rare location for lipomas.[1] The lesion’s location influences the clinical features of intraoral lipoma. Oral lipomas are more commonly located in the buccal mucosa, which contains abundant adipose tissue due to the nearby buccal fat pad.[2,3] Other commonly involved sites include the tongue, floor of the mouth, palate, lips, vestibule, mandible and retromolar pad. Angiolipoma, a histopathological subtype of lipoma, characterised by intermingled adipose tissue and vascular components, has been rarely reported in oral cavity.[4]
A 43-year-old male presented with complaint of painless swelling on inner lower lip mucosa for the past 1 year with a progressive increase in size, It was associated with some discomfort while swallowing food and talking. The lesion was not associated with pain, bleeding or episodes of rupture and discharge from swelling or change in size while eating. On examination, a single well-defined swelling 1 cm in diameter was seen on lower lip mucosa, which was soft, mobile, non-fluctuant, non-tender with normal overlying mucosal surface [Figure 1a]. Lymph nodes were not palpable in submental, submandibular, upper, middle and lower jugular region or in post triangle. Differential diagnoses of oral lipoma, mucocele and benign salivary gland tumour were considered and the patient was sent for fine needle aspiration cytology but no fluid could be aspirated. Surgical excision done under local anaesthesia showed a single encapsulated yellow-white soft-tissue mass of size 1 × 1 cm, soft to firm in consistency which was excised and sent for histopathological examination [Figure 1b]. The histopathology reported it as angiolipoma, showing partly encapsulated tumour made of mature adipose tissue partitioned by fibrous septa and hyaline globules in blood vessels [Figure 1c].
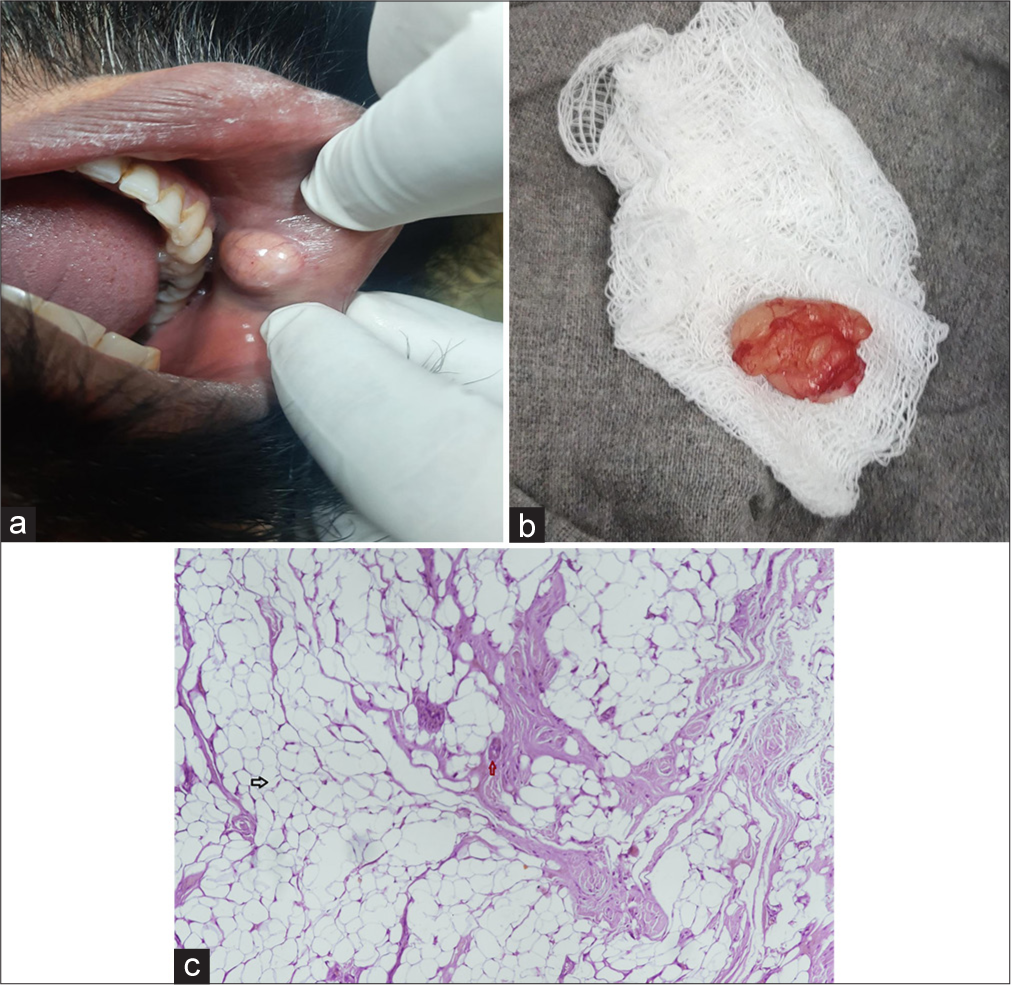
- (a) A single well-defined swelling 1 × 1 cm on lower lip mucosa, soft, mobile, non-fluctuant, non-tender with normal overlying mucosal surface, (b) yellow-white soft-tissue mass of size 1 × 1 cm, soft to firm in consistency, (c) histopathological examination using haematoxylin and eosin stain at 40x maginification showing mature adipose tissue (black arrow) and hyaline globules in blood vessels (red arrow).
The increasing heath awareness among people has led to early diagnosis and treatment in variety of diseases, though there is increased fear of minor health aliments being cancerous. Any swelling or lump seen to felt by the patient is feared to be cancerous and same is true for oral swellings. Intraoral swelling can be caused by mucocele, dermoid and epidermoid cysts, lymphoepithelial cysts, benign salivary gland tumours, benign mesenchymal neoplasms, ranulas, lymphoma, ectopic thyroid tissue and lipomas. Lipomas are the most common benign mesenchymal tumours originating from mature adipocytes, commonly found in trunk and proximal extremities. Their occurrence, however, in head-and-neck region is rare and in oral cavity all the more infrequent.
The various aetiopathogeneses for the development of oral lipomas include ‘Hypertrophy theory’ stating that obesity causes inadvertent adipose tissue growth. However, this theory does not explain the occurrence of these lesions in areas devoid of pre-existing adipose tissue.[5] ‘Metaplasia theory’ states that in situ mesenchymal cells differentiate into lipoblasts which lead to lipomatous tissue formation. Chronic irritation and trauma may also trigger proliferation of soft tissue, causing lipoma formation.
Intraoral lipomas most commonly occur in the buccal mucosa, with other frequent sites including the tongue, lips, floor of the mouth, palate and gums. This corresponds to amount of fat present in these tissues. They usually present as well-defined, round-to-oval submucosal nodules of size ranging from 0.2 cm to up to 5 cm. Symptoms include discomfort, feeling of fullness, difficulty in speech, mastication and dysphagia. Multiple lipomas have been associated with certain syndromes such as Gardner’s syndrome, multiple subcutaneous lipomas, Decrum’s disease, encephalocraniocutaneous lipomatosis, multiple familial lipomatosis, neurofibromatosis and proteus syndrome.
Microscopically, lipomas are classified into several types, including classic lipoma, sialolipoma, angiolipoma, spindle cell lipoma, fibrolipoma as well as pleomorphic, myxoid and intramuscular lipomas. Angiolipomas composed of mature adipocytes and blood vessels account for 5–17% of lipomas. They are further classified into non-inflitrating and inflitrating variant. Although benign, incomplete excision of inflitrating variant can lead to recurrence. The presence of blood vessels inside the lesion and high vascularity of oral mucosa together increase the risk of bleeding during excision. Surgeon should therefore bear in mind the need for haemostasis.
Angiolipomas, though rare in oral cavity, have an excellent prognosis, as no malignant potential has been reported. However, if not excised, these do not regress spontaneously and continue to increase in size and become cosmetically disfiguring.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Lipomas and Fibrolipomas of the Oral Cavity. J Maxillofac Surg. 1982;10:177-81.
- [CrossRef] [PubMed] [Google Scholar]
- Oral Lipoma: Analysis of 58 New Cases and Review of the Literature. Ann Diagn Pathol. 2011;15:257-61.
- [CrossRef] [PubMed] [Google Scholar]
- Lipoma of the Oral and Maxillofacial Region: Site and Subclassification of 125 Cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:441-50.
- [CrossRef] [PubMed] [Google Scholar]
- Noninfiltrating Angiolipoma of the Cheek: A Case Report and Review of the Literature. J Oral Sci. 2009;51:137-9.
- [CrossRef] [PubMed] [Google Scholar]






